Summary
[W]e should never, ever see cervical cancer. Not in the United States. I had a lady two years ago, she had no money and came up here because she was having spotting after intercourse for two years. Hadn't had a pap test in 10 years. She'd been to the emergency room three times [for it].... So, when she came in here, I told her I'd look at her. Put [in] the speculum and she had cervical cancer coming down her vagina. 27 years old.
—Dr. William M. Stevens, obstetrician gynecologist, Selma, Alabama, April 11, 2018.
Cervical cancer deaths should not happen. This cancer is ultimately preventable and highly curable. The later the disease is diagnosed, the more likely it is to be a death sentence. Dr. Stevens, who has been practicing for over 30 years, says the case he refers to above is not an exception. He compares the situation in Alabama’s deprived Black Belt to that in an under-resourced rural community in Kenya where he also runs a clinic. “I see things that are bad here.”
The Alabama Black Belt is a stretch of counties, historically defined by rich black soil and now known for its primarily African American population, high rates of poverty and poor physical health. Because there are few gynecologists in those counties, Dr. Stevens’ office is one of the closest gynecological referral sites for five or six counties, some of which are among the poorest in the state. Perry County, where Frances F. lives, is one of those counties. Frances’s mother died from cervical cancer. This happened over three decades ago, when she recalled that Perry County had a hospital but no gynecologist. Today it has neither. Early intervention could have saved her mother’s life, but something held her back. “She knew something was wrong,” Frances told Human Rights Watch. “She didn’t know what, but she didn’t stop to take care of herself…. People didn’t talk about things like that. They were afraid. ”
Advances in medical technology have sent cervical cancer mortality rates plummeting in nations with developed heath care systems. Yet about 4,200 women in the US will die from cervical cancer this year. In Alabama, women are dying from the disease at rates that are higher than in any other state in the US. Black communities are particularly impacted. Nationwide, Black women are more likely to die from this disease than women from any other racial or ethnic group.
This is significantly, though not exclusively, a problem of state neglect of women living in poverty. State policies and law, together with recent federal changes, limit the effectiveness of the few state and federal resources that exist to help make reproductive health care services and information accessible to low-income Alabamian women.
Racial inequality, historically embedded in the Alabama health and education systems, has made the situation worse for many poor women. Black Alabamians are twice as likely to live in poverty as white Alabamians. Moreover, racial disparities in cervical cancer deaths are not reducible to disparate income levels. Studies have found that even when Black women with cervical cancer earn as much as white women, they are still at higher risk of death from the disease. And yet, the state fails to support programs that could address the negative impact of substantial barriers, such as reticence to seek out reproductive health care, that interviewees in the Black Belt told Human Rights Watch impacts cervical cancer care in their communities.
There are four points of intervention that can prevent, treat, or cure cervical cancer so that woman do not die from it. The human papillomavirus (HPV) vaccine prevents women and girls from contracting HPV, a very common sexually transmitted infection that causes the vast majority of cervical cancer cases. Cervical cancer screenings detect early changes in cervical cells. Timely follow-up after abnormal screenings ensures that precancerous lesions are removed before they can develop into cancer. Finally, cervical cancer, when detected in its early stages, can be effectively treated with a high survival rate. At each point, access to sexual and reproductive health information and comprehensive sexual health education can give women and girls the tools necessary to make informed decisions about decreasing cervical cancer risk.
Alabama’s high rates of cervical cancer deaths suggest that the health system is failing some women at one or more points. Between November 2017 and April 2018, Human Rights Watch spoke to more than 100 women, medical experts, service providers and others, to try to understand how and where the state and others fail to provide women the care they need. This report presents the voices of some of the women living in the Alabama Black Belt and highlights how state and federal policies neglect some of the most vulnerable communities in the state, contributing to circumstances that are ripe for preventable cervical cancer deaths.
In a troubling trend, the percentage of women screened for cervical cancer has been decreasing nationwide and statewide over time. Nevertheless, Alabama’s screening rates are consistently above the national average and Black Alabamian women in particular are accessing screenings at higher rates than white Alabamian women. The persistent racial disparities in death rates, therefore, defies evidence that more cervical cancer screenings mean fewer cervical cancer deaths. The problem—the failed points of intervention that most contribute to Black women being two times more likely to die from cervical cancer than white women—comes both earlier and later in the continuum of care. Alabama’s greatest missed opportunity is in the beginning, in its failure to ensure women and girls have access to preventive services and quality sexual and reproductive health information. The state’s greatest access flaw is later in the cervical cancer care continuum, after screening, in follow-up delays and treatment differences.
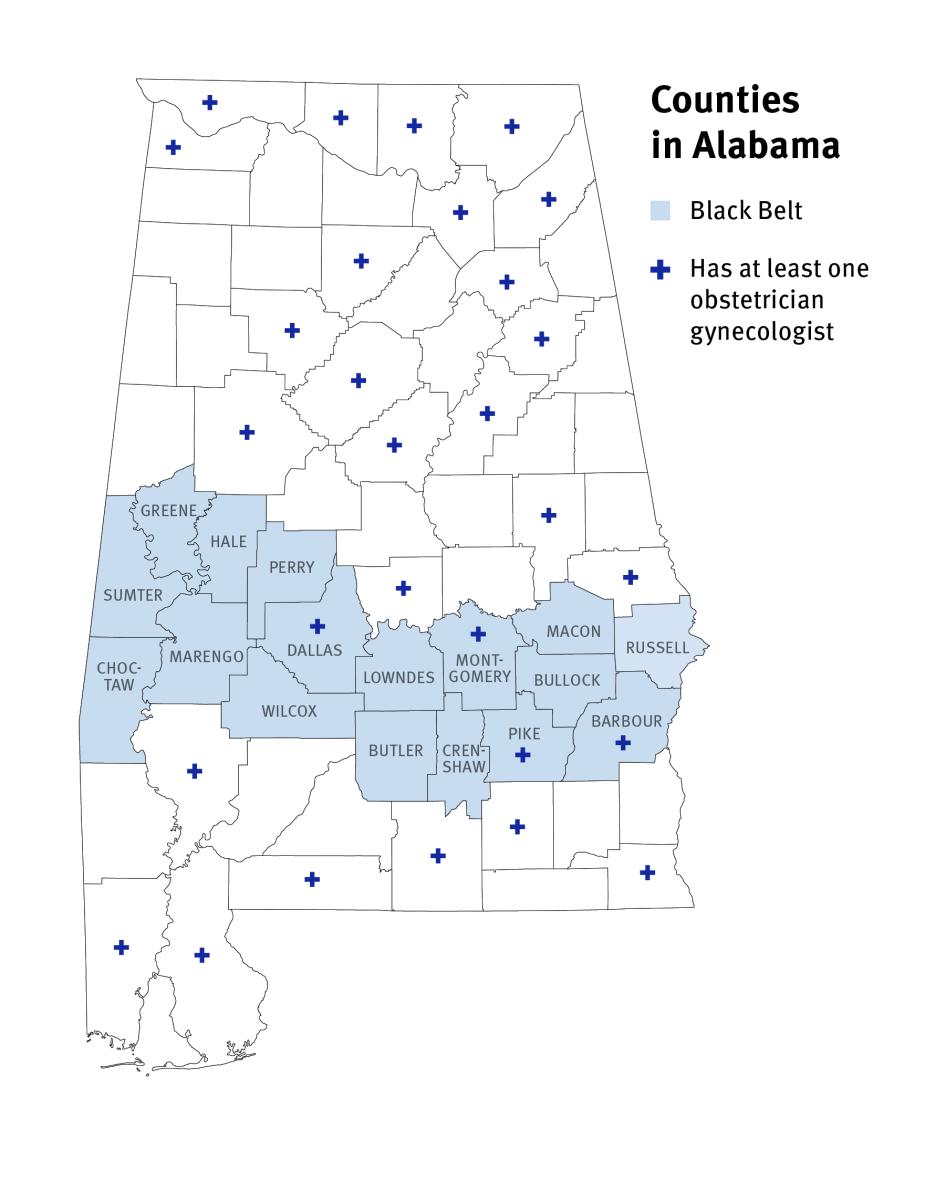
For women living in the Alabama Black Belt, obtaining reproductive health care often disrupts their lives in small and large ways. Human Rights Watch found that a vast majority of Black Belt counties have no gynecologist and most women have to drive, or pay someone to drive, long distances in order to have simple procedures such as follow-ups from abnormal cervical cancer screenings. For instance, Darcy C., 57, pays up to US$150 for the two-and-a-half-hour trip to her gynecological oncologist for cervical cancer screenings and other tests. Darcy C., told Human Rights Watch, “It’s really hard. And I have to go without a lot to make sure that I have the money…. I get barely $700 per month, so with the bills I have to pay, it doesn’t leave anything for a trip.”
The cost and burden of travel for care can compound pre-existing financial constraints and contributes to the need to make difficult decisions. Women described having to choose between reproductive health care and other basic needs such as electricity, medication, and healthy food. Inconsistent health care coverage compounds the problem. Women told Human Rights Watch that they avoided non-emergency health care while uninsured, which, for some, meant that gynecological cancers weren’t found until symptoms developed to more advanced stages—making the women less likely to be cured.
State and Federal Policies Help Sustain Barriers to Obtaining Cervical Cancer Care
The Alabama public health care system is not structured to ensure consistent access to care for poor women. Alabama, along with Texas, has the lowest Medicaid eligibility levels in the nation. Able-bodied adults who are not pregnant or caregivers are completely ineligible for full Medicaid, no matter how poor. A patchwork of additional programs targets specific health care concerns, but each program has coverage limitations and unique, sometimes fluctuating, eligibility criteria. Funding limitations further inhibit access to care. The only program designed to link uninsured women to cervical cancer care is debilitated by financial constraints. It is reaching fewer than one in five eligible women and program staff are not doing more outreach for fear of outstripping funds if uptake increases. The piecemeal approach to health care leaves broad coverage gaps and some poor women have no option but to pay out-of-pocket for cervical cancer related services or forego them altogether.
The state could ensure better and more consistent access to preventive and primary health care services for women who are below or near the federal poverty level by expanding Medicaid eligibility. In choosing not to do so, Alabama is leaving federal money on the table and going against the recommendation of a state taskforce on healthcare improvement. Instead of facilitating access to health care for Alabama residents, state and federal governments have taken steps to make it more difficult by threatening to add work requirements for Medicaid and by weakening obligations that health plans include essential benefits such as preventive services. Additionally, restrictive state reproductive health policies make it more difficult for women to obtain abortion care and control cervical cancer risk factors like having multiple children and giving birth at a young age.
Alabama’s obstetrician gynecologist shortage has created a crisis in access to reproductive health care services. The state’s patchwork approach to public health care and failure to expand Medicaid have helped prolong this crisis. Expanding Medicaid eligibility to more people would raise insurance coverage rates and decrease uncompensated care for hospitals, which in turn would help stem the high number of rural hospital closures in the state. Without positive action from the state, rural hospitals will continue to be at risk of shutting down. Obstetrician gynecologists need hospitals in order to provide services such as maternity care; therefore, when hospitals close, obstetrician gynecologists move away. Insufficient Medicaid reimbursement rates also means some gynecologists will only accept a limited number of Medicaid patients, leaving women on public programs with even fewer options.
Other factors, such as dwindling rural populations and providers’ personal preferences regarding where to live and practice contribute to these problems as well. But government inaction plays a significant role, and the policies and government choices highlighted in this report help to make cervical cancer care even more difficult for rural women to obtain. Such harmful choices include: maintaining a patchwork system of social safety net care that does not ensure consistent coverage for cervical cancer related services, declining to expand the Medicaid program to cover more low-income people, enacting regulations that target abortion providers and inhibit access to abortion care, failing to appropriate state funds for public transportation, and having significant gaps in access to reproductive health related information including maintaining non-comprehensive sexual health education that is voluntary for schools to offer.
Alabama has the chance to give women the tools to decrease their cervical cancer risk. Quality information about sexual and reproductive health is indispensable to making informed decisions about cervical cancer related care, but women, providers, and local advocates, reported severe problems with access to information. The HPV vaccine, which is recommended for children ages 11 to 12, could prevent a vast majority of cervical cancer cases. And yet some parents with children are never told about the vaccine. Others did not know that they could access free or low cost cervical cancer related services from the public health department. Moreover, Human Rights Watch found that some women did not receive any, let alone comprehensive, sexual health education in school.
Failures in provider communication and public outreach contribute to the access to information problem. So, too, do Alabama’s education policies. Many Alabama counties struggle to fund their public schools, and Black Belt counties face particular challenges in raising local funds because of restrictions under the state constitution. In the context of an already underfunded school system, sexual health education is left unregulated and unmonitored. This is a problem for cervical cancer prevention efforts because the disease is largely caused by HPV, a sexually transmitted infection. The state does not require schools to provide sexual health education, but if they chose to do so, they are statutorily required to place a heavy emphasis on abstinence and stigmatize homosexuality.
The failure to guarantee equal access to comprehensive sexual health education disadvantages some students more than others. In practice, only half of the schools in the state teach high school students how to obtain condoms and fewer than half teach them how to use condoms correctly. This leaves some students without information necessary to prevent HPV and lower cervical cancer risk. Moreover, the highest rates of new chlamydia infections and prevalence of HIV in the state are clustered in Black Belt counties.
In addition to state and federal policies, historical memory and harmful social norms can make it difficult to connect some women to care. Alabama’s Black Belt is the site of the unethical Tuskegee syphilis experiments, and federally funded coerced sterilizations of many poor, and primarily Black, women and girls.
Women described how other barriers, such as fatalistic attitudes about cancer survival or unwillingness to talk about sex, negatively impacted their willingness to seek out reproductive health care. For example, one health care provider said that patients sometimes refuse Papanicolaou (Pap) tests because, as they’ve told her, “I’m going to die from something.” Other interviewees relayed how past experiences like feeling neglected or judged by health care providers have contributed to distrust of the public health department and alienation from the health care system generally.
The challenge to the Alabama Department of Public Health (ADPH) of reaching women who cannot or will not seek out reproductive health care is not simple. However, the gaps in access to information and education in the state help these barriers to continue to impede access to reproductive health care. Programs that prioritize community engagement and education can help disrupt harmful social norms, connect women to care, and reduce health disparities in cervical cancer outcomes. There is an established network of community health advisors in the Alabama Black Belt who work to do precisely this.
The community health advisor (CHA) program in the Black Belt was federally funded for over a decade, but activities largely ended in August 2016 after the last grant cycle ended. A skeletal network of community health advisors continued in 7 of the original 22 counties with the help of state funds through the Alabama Breast and Cervical Cancer Early Detection Program (ABCCEDP). The goal was to take advantage of community-based cancer prevention networks that already existed, but nevertheless the state recently stopped providing even minimal funds to the program in the Black Belt. Without any public support, the program must find private funding sources or its networks are at risk of collapse.
State and Federal Governments Fail to Protect Alabamian Women’s and Girls’ Rights to Health, Information, and Non-discrimination in Relation to Cervical Cancer Care
Women have the right to access full and comprehensive sexual and reproductive health related information and services, without discrimination, to make informed decisions about their bodies and reproductive futures.
The International Covenant on Economic, Social and Cultural Rights (ICESCR) recognizes “the right of everyone to the enjoyment of the highest attainable standard of physical and mental health.” The US has signed, but not ratified, that treaty. The Universal Declaration of Human Rights (UDHR), which has the endorsement of all United Nations member states and is considered broadly reflective of customary international law, also articulates the right to health.
The UN expert on extreme poverty has recently issued a report that is sharply critical of US polices in this area, and asserts that efforts to undermine the Patient Protection and Affordable Care Act (ACA) “by stealth” are an abuse of the right to health.
Women and girls have a right to access health-related information under numerous human rights treaties. The International Convention on the Elimination of All Forms of Racial Discrimination (ICERD), which the US has ratified, also obligates governments to address not only intentional racial discrimination but laws, policies and practices that result in a disparate racial impact, including in relation to public health.
The state and federal governments have allowed substantial barriers to comprehensive cervical cancer care to continue to impede care in Alabama, and in doing so, have failed to protect women’s rights to health, information, and non-discrimination.
The root causes of persistent reproductive health disparities are complicated. The government action and inaction highlighted in this report help explain persistent racial disparities in cervical cancer death rates in Alabama and shed light on why women in the state die from cervical cancer at rates higher than any other US state. To effectively address the cervical cancer problem, Alabama needs to confront how persistent racial and socioeconomic inequality in health care access and education negatively impacts women. Alabama should take concrete steps to reduce racial disparities in cervical cancer outcomes by expanding Medicaid to close the coverage gap in Alabama; repeal restrictions on reproductive health care that make it more difficult for women to control cervical cancer risk factors; appropriate funds for public transportation; reform its sexual health education law; enact policies that address gaps in access to reproductive health related information, such as supporting and expanding community-based approaches to cervical cancer prevention.
Until federal, state, and local authorities invest in programs and policies that support equal access to comprehensive sexual and reproductive health care services and information, women from vulnerable and marginalized communities, such as poor and African American women, in the US and in Alabama will continue to die disproportionately from preventable cervical cancer deaths.
Recommendations
To the Alabama State Government
To the Governor of Alabama
- Support the expansion of Medicaid under the federal Patient Protection and Affordable Care Act to increase access to medical services for the residents of Alabama.
- Withdraw the Section 1115 Demonstration proposal from US Health and Human Services, which would require unemployed or underemployed able-bodied parents or caretaker relatives to become gainfully employed or to participate in employment-related activities in order to be eligible for Medicaid.
- Develop a comprehensive and costed plan to eliminate cervical cancer deaths in Alabama and work with the legislature to fund it.
To the Alabama State Legislature
- Pass legislation to expand Medicaid under the federal Patient Protection and Affordable Care Act in order to increase access to medical services for the residents of Alabama.
- Appropriate funds for cervical cancer prevention, treatment, and maintenance care.
- Support community health outreach programs.
- Abolish statutory requirements in Alabama Code for sexual health education which are not based on scientific evidence and replace them with requirements for scientifically and medically accurate, comprehensive sexual health education; and adopt legislation, like the Alabama Youth Health Protection Act (SB269), that brings state law in line with federal standards. The curriculum should address sexually transmitted infections and effective methods of protection without stigmatizing or shaming safe, sexual behavior and should not be exclusive of any specific sexual orientation, gender or gender identity, and ensure funding for the implementation of the curriculum.
- Ensure state law does not restrict or undermine access to necessary and life-saving women’s health care. Develop programs to address barriers to accessing health care services linked to the unavailability of public transportation.
- Take effective steps to ensure counties and cities can adequately fund their schools and meet local needs, including funding for scientifically and medically accurate, comprehensive sexual health education.
- Repeal Section 256 of the Alabama Constitution mandating that the state maintains “separate schools for white and colored children”, which has contributed to the poor health and wellness of the parts of Alabama left isolated as de jure has turned to de facto segregation.
To State Agencies Including the Alabama Department of Public Health, the Alabama Department of Education, and Alabama Medicaid
- Track compliance rates for follow-up colposcopies and diagnostic testing in order to better assess areas and populations that are most vulnerable.
- Deploy reproductive health and cervical cancer resources to areas where there is the least coverage.
- Support community health workers and community-based approaches to reproductive health care that address health care access and the social determinants of health.
- Conduct a public awareness campaign in full collaboration with local and community mobilization groups about:
- Services offered by county health departments.
- Cervical cancer prevention care, including how to access services that can help reduce cervical cancer risk.
- Increase targeted outreach, awareness-raising and provider trainings to ensure high coverage for the HPV vaccine, taking into consideration the new US Food and Drug Administration (FDA) approval for individuals through the age of 45.
- Establish inclusivity policies that:
- Support linguistic and racial diversity, including in county public health departments.
- Acknowledge, confront, and seek to remedy historic and current experiences of racial discrimination.
- Create an official complaint mechanism for patients who use the public health departments and for providers who participate in programs such as the Alabama Breast and Cervical Cancer Early Detection Program and Plan First program.
- Continue the process of implementing electronic medical records.
To the United States Government
To the President of the United States
- Withdraw executive orders that could undermine or weaken the ACA, such as the Executive Order Minimizing the Economic Burden of the Patient Protection and Affordable Care Act Pending Repeal and the Executive Order Promoting Healthcare Choice and Competition Across the United States.
- Approach the US Senate to ratify the International Convention on Economic, Social and Cultural Rights, the Convention on the Elimination of all forms of Discrimination against Women, and the Convention on the Rights of the Child.
To Congress
- Pass legislation aimed at addressing high rates of preventable cervical cancer deaths including racial disparities in mortality rates.
- Expand the National Breast and Cervical Cancer Treatment program to provide for maintenance care for women who have been successfully treated for breast or cervical cancer.
- Provide consent to the International Convention on Economic, Social and Cultural Rights, the Convention on the Elimination of all forms of Discrimination against Women, and the Convention on the Rights of the Child.
- Stop all efforts to repeal the ACA and reinstate the individual mandate to secure the long-term viability of the ACA marketplace.
- Support Medicaid expansion into all states as an important measure for addressing preventable gynecological cancer deaths.
To Federal Agencies including the US Centers for Disease Control and Prevention and the Department of Health and Human Services
- Withdrawal regulations that undermine or weaken the ACA, such as sections of the Health and Human Services (HHS) Notice of Benefit and Payment Parameters that would weaken the essential health benefits mandate.
- Restore advertising and outreach funds for open enrollment for the ACA Marketplace.
- Restore or recommit to providing federal funding to cost-sharing reduction payments.
- Reject Alabama’s Section 1115 Demonstration proposal on Medicaid workforce initiative, which would require unemployed or underemployed able-bodied parents or caretaker relatives to become gainfully employed or participate in employment-related activities in order to be eligible for Medicaid.
- End the trend of prioritizing abstinence-only education grants and return to the past policy of funding comprehensive sexual health education programs.
- Recommend that colposcopy, diagnostic testing for cervical cancer and precancerous lesions, and early interventions like excisional and ablative treatments, all of which help in the prevention of cervical cancer, be included as a preventive care under the ACA’s essential health benefits mandate.
- Review and adjust the current methodology for cervical cancer data analysis to ensure that it reflects the true rates of cervical cancer incidence and mortality. The review should consider whether including women with hysterectomies in the at-risk population artificially lowers racial disparities in cervical cancer rates.
To National, State and Municipal Authorities Across Sectors
- Elicit feedback from communities and populations that are disproportionately impacted by cervical cancer death about their needs.
- Encourage gender, age, racial, ethnic, and linguistic diversity in the relevant public and private sector, including in the health care and education systems.
To the United Nations
To the United Nations Committees on Human Rights and the Elimination of Racial Discrimination
- Call upon the United States to comply with its international obligations to eliminate disparate racial impacts in public health including the disparate racial impact of cervical cancer.
- Call upon the United States to improve oversight, establish incentives, and take other necessary steps to ensure compliance with human rights obligations at the state and local levels.
Methodology
This report is based on individual and group interviews conducted with a total of 63 women in Alabama between January and April 2018. Group or individual interviews were conducted with 57 women who identified themselves as Black or African American.[1] Five interviews were with women who identified themselves as Latina. The individual and group interviews were concentrated in seven counties in the western portion of the Alabama Black Belt and two counties in Central Northern Alabama.
Individual interviews were conducted with 32 women between the ages of 20 and 79. Most were in person but, because of transportation difficulties, nine took place over the phone. Human Rights Watch held interviews individually and in private when possible but some interviewees preferred to have another person present. Twelve interviews were conducted with a Human Rights Watch researcher and a research partner from the community. Interviews were primarily held in homes or community spaces.
Our interviews focused on women’s experiences obtaining cervical cancer related care. The interviews often touched more broadly on the reproductive health care needs and experiences of women of color living in rural Alabama. Three interviewees had a personal experience with cervical cancer, either as a survivor or through the loss of a family member, and three had another type of gynecological cancer. Additionally, six of the women interviewed received hysterectomies due to a gynecological problem.
Human Rights Watch also consulted with or interviewed a total of 57 academics, medical providers, public health officials, lawmakers, and representatives of civil society or non-governmental organizations, including 21 medical providers, public health officials, and experts, about their experience with cervical cancer related care and 20 representatives from organizations working in the Alabama Black Belt.
Human Rights Watch did significant background research and quantitative data analysis of secondary sources for this report. A Human Rights Watch researcher compiled data through publicly available sources and information requests through Alabama’s public records law. Specifically, Human Rights Watch requested aggregate data about cervical cancer statistics from the Alabama Department of Public Health (ADPH) and the Alabama Breast and Cervical Cancer Early Detection Program (ABCCEDP). Any known limitations on data reliability are noted and all documents relied upon are referenced or on file with Human Rights Watch.
All interviewees provided verbal informed consent. They were told that they could end the interview at any time or decline to answer any questions without negative consequences. All participants were informed of the purpose of the interview, its voluntary nature, and the ways that information would be collected and used. In cases where interviewees requested that their name remain confidential, Human Rights Watch has used a pseudonym in this report.
Human Rights Watch did not provide anyone with compensation for participation. Interviews lasted anywhere from 15 minutes to over an hour, depending on the availability of the interviewee. For those that were an hour or more, light refreshments such as snacks and water were offered. For group interviews conducted over meal times, Human Rights Watch provided a modest meal.
Interviews were primarily conducted in English. Three were conducted in Spanish by a Human Rights Watch senior researcher. Human Rights Watch identified interviewees through collaboration with community research partners and with the assistance of local organizations that have connections with women in their communities.
There are multiple definitions of which counties constitute the Alabama Black Belt region. Unless otherwise noted, this report relies on the traditional definition of the 17 counties stretching across central Alabama: Barbour, Bullock, Butler, Choctaw, Crenshaw, Dallas, Greene, Hale, Lowndes, Macon, Marengo, Montgomery, Perry, Pike, Russell, Sumter, and Wilcox.
I. Cervical Cancer Is Preventable and Curable
No one should die from cervical cancer. It is preventable and highly curable, with a 93 percent survival rate when detected early.[2] There are four points at which a state, through its health and education systems, can intervene to reduce mortality from the disease: prevention (including education and preventive services), screening, follow-up, and treatment. Most cervical cancer deaths in the US can be attributed to failures at one or more of these junctures.[3]
Cervical cancer is one of the most common cancers in women worldwide and in dozens of countries it kills more women than any other form of cancer.[4] The burden of this disease is not evenly distributed. Inequality—including inequality in income, in access to education and services, and based on marginalized status—is a powerful driver. Almost nine out of every ten women who died from cervical cancer worldwide in 2012 came from low-income to middle-income countries.[5] The gaping disparity can be explained by stark differences in access to effective prevention, early detection, and treatment programs. It is fueled in part by what the World Health Organization has called a “shocking neglect” of women in low- and middle-income countries.[6]
Cervical cancer deaths in the US occur primarily in certain marginalized pockets. Women who are poor, uninsured, or lack regular access to health care die at much higher rates than the average population. Black women, and particularly older Black women, are especially vulnerable and according to data are dying of cervical cancer at rates that some specialists believe are as high as in Sub-Saharan Africa.[7]
This section provides background on the four points of intervention where a cervical cancer death could be prevented: vaccination, screening, timely follow-up, and early treatment. The fact that many women continue to die from cervical cancer indicates that they are being failed at one or more of these points.
The HPV Vaccine Can Help Prevent the Spread of the Virus That Causes Cervical Cancer
The HPV vaccine is a first layer of defense against cervical cancer.[8] Nearly all cases of cervical cancer are caused by persistent infection with human papillomavirus (HPV), a very common virus that spreads through sexual contact.[9] Most HPV infections clear within a year or two, but those that do not could lead to cervical precancerous lesions (abnormal cervical cells that could develop into cancer) or cancer.[10]
Gardasil 9 is the only HPV vaccine available in the US.[11] It radically decreases the chance of developing cervical cancer by protecting against the strains that are responsible for 75 to 90 percent of all cervical cancer cases.[12]
The vaccine is approved by the federal Food and Drug Administration (FDA) for males and females ages 9 to 26.[13] As of October 2018, this FDA approval extends to individuals 27 to 45 years old.[14] The Centers for Disease Control (CDC) recommends routine vaccination for children who are 11 or 12.[15] It is important to vaccinate children before they become sexually active in order to develop immunity before exposure to the HPV virus.[16]
To be effective, boys and girls ages 9 to 14 should receive 2 shots within 6 months to a year of each other.[17] Anyone who initiates the series between the ages of 15 and 16 should receive 3 doses, the second 1 to 2 months after the first and the third 6 months after that.[18] The consequence of a complicated vaccination protocol is that not everyone completes it. In 2016, for instance, 60.4 percent of adolescents ages 13 to 16 initiated the HPV vaccine, but only 43.4 percent completed the series.[19] Vaccination rates have been improving in the US, but still fall well below the federal government’s goal of an 80 percent vaccination completion rate.[20]
The vaccine immunizes against many, but not all, high-risk strains of HPV and there are many women, men, girls, and boys, who could not or did not complete the vaccine before becoming sexually active. Even if vaccination rates increased dramatically in the coming years, screening and other secondary preventive measures would still be necessary.[21]
Screening and Timely Follow-up Treatment Can Prevent Cervical Cancer from Developing
Together, routine screening and timely follow-up are an effective method for preventing cervical cancer. The former detects cervical cell changes and the latter removes the potentially dangerous cells before they can turn into cancer. In the early 1900s cervical cancer was the number one cancer-related cause of death for women in the US, but the introduction of testing helped that number plummet.[22]
There are two types of cervical cancer screening tests: the Papanicolaou (Pap) and the HPV test.[23] The Pap test was introduced in 1942 and led to the rapid decline of cervical cancer incidence and mortality; rates declined by more than 60 percent between 1955 and 1992.[24] In 2003, the first HPV test was FDA approved in the US.[25] Both are still used today.
These tests identify cervical cells that could develop into cancer but they do not diagnose or treat cervical cancer or precancerous lesions.[26] If a test returns an abnormal result, the next steps differ depending on what kind of abnormal result was returned.[27] The changes to cervical cells could be low-grade, high-grade, or of an undetermined significance.
Oftentimes, low-grade changes are caused by an HPV infection that will resolve on its own and may only require monitoring with a repeated Pap or HPV test in one year.[28] Additional screening can generally be done at the same office that did the original test. If the low-grade changes are accompanied by a positive HPV test, the provider might recommend a colposcopy—a procedure to more closely examine the cervix for abnormal changes.[29] High-grade changes are more likely to be associated with precancerous lesions or cancer and indicate that more aggressive follow-up, such as a colposcopy, biopsy, or treatment, may be necessary to prevent cervical cancer.[30]
In practice, most colposcopies are performed at a gynecologist’s office or at a colposcopy clinic.[31] Roughly eight percent of patients screened for cervical cancer will be referred to a specialist due to an abnormal screening test.[32] Sometimes, if a patient shows symptoms of cervical cancer such as post-coital bleeding, they may be referred to a gynecologist for a colposcopy without even a Pap test.[33]
If the colposcopy confirms abnormal cells, the provider might biopsy the area and send the sample for testing to determine whether cancer or precancerous cells are present.[34] They might also perform excisional or ablative treatment, which remove or destroy the abnormal tissues.[35]
Cervical Cancer Is Highly Curable with Early Detection and Prompt Treatment
Cervical cancer progresses slowly: it generally takes about 10 to 15 years for HPV to develop into cervical cancer.[36] The slow progression is a large reason why cervical cancer is relatively easy to prevent and, when detected early, to treat.
Cervical cancer diagnoses range from stages 0 to IV. Stage 0 is called noninvasive cervical cancer or “carcinoma in situ.” At this stage, cancer cells are only on the top layer of the cervix. Stages I and beyond are considered invasive.
A number of factors can influence the treatment protocol, including the stage of the tumor, comorbid conditions, and personal preferences, but generally invasive cervical cancer is treated with surgery, radiation, chemotherapy, or some combination thereof.[37] Once cervical cancer is in remission, regular maintenance appointments, including physical exams, lab tests, and scans, are important to ensure that women remain cancer-free.[38]
The five-year survival rate for cervical cancer varies widely according to staging. The chance of survival drops alarmingly for later-stage diagnoses. Women diagnosed with local, early stage cervical cancer have a 93 percent five-year survival rate.[39] That falls to 15 percent in the last stage, when the disease is generally no longer considered curable.[40]
|
Cervical cancer stages, treatment options and survival rate |
|||
|
Stage |
Subdivision |
Indicated Treatment37 |
Survival Rate38 |
|
Stage I: tumor is confined to the cervix |
IA: Small amount of cancer can be seen with a microscope |
Excision; total hysterectomy; radical hysterectomy; internal radiation therapy; external beam radiation therapy plus brachytherapy; radical trachelectomy (removal of cervix but not uterus) where preservation of fertility is desired. |
93% |
|
IB: Cancer is visible without a microscope |
Radical hysterectomy; high-dose internal and external radiation therapy; radical trachelectomy; combination of chemotherapy and radiation therapy |
80% |
|
|
Stage II: spread beyond the cervix but not to the pelvic side wall. |
IIA: Cancer has spread to the upper two-thirds of the vagina but not to the uterus |
Internal and external radiation therapy; radiation therapy plus chemotherapy; radical hysterectomy followed by radiation therapy and chemotherapy |
63% |
|
IIB: Cancer has spread to both the vagina and uterus |
Combined internal and external radiation therapy along with chemotherapy with cisplatin; other drugs along with cisplatin |
58% |
|
|
Stage III: cancer has spread to the lower third of the vagina. |
IIIA: Cancer has not spread to the pelvic wall |
Combined internal and external radiation therapy plus chemotherapy |
35% |
|
IIIB: Cancer has spread to the pelvic wall and may block proper kidney function |
Combined internal and external radiation therapy plus chemotherapy |
32% |
|
|
Stage IV: advanced (metastasized) cancer: has spread to other organs or regions of the body. |
IVA: Spread to local organs such as the bladder or rectum |
Combined internal and external radiation therapy plus chemotherapy |
16% |
|
IVB: Spread beyond pelvic area to other areas such as the liver, intestinal tract, or lungs |
Generally, not considered curable. Radiation therapy and/or chemotherapy to relieve symptoms and improve quality of live |
15% |
|
II. Cervical Cancer Deaths in Alabama Reflect Inequality and Neglect in the Health System
The US has the medical and technical expertise to prevent cervical cancer deaths.[41] In the US, cervical cancer was once the most common cancer and cause of cancer death in women.[42] Now, it is not even in the top 10 for incidence or mortality.[43] With sufficient government support, the disease could feasibly be eliminated.
Yet in 2015, according to the most recent numbers available from the Centers for Disease Control and Prevention, 4,175 women in the US died from cervical cancer.[44] Even conservatively, this is at least five times the number of women who died from pregnancy-related or delivery-related complications.[45] Worse, the mortality rate has stopped declining and slightly more women are predicted to die from cervical cancer in the US in 2018 than in 2014. The United Nations expert on extreme poverty recently sharply criticized the US and cited cervical cancer as one example of how persistent racial discrimination has made the burdens of poverty even worse for many women.[46]
No one should die from cervical cancer, but some groups—those that are traditionally marginalized or vulnerable in the US—do more often than others. For Black women, poor women, women without insurance or regular access to health care, and those who fall into more than one of these categories, cervical cancer is more likely to be a death sentence. Such disparities in death rates reflect the inequality that is embedded in the US health and education systems.
Black Women Die from Cervical Cancer at Higher Rates Than Any Other Racial or Ethnic group
Cervical cancer is a disease of inequality. Poverty, lack of insurance, lack of regular access to health care, and low education levels are all powerful drivers of cervical cancer risk—something that it has in common with many other preventable diseases and conditions.[47] Economic deprivation is strongly and independently associated with cervical cancer mortality and women from poor communities have a higher risk of late-stage diagnosis and lower rates of cervical cancer survival than those from more affluent communities in the US.[48] Individuals with public or no insurance are less likely to be screened, more likely to have a late-stage diagnosis, and obtain optimal treatment less frequently.[49] Moreover, Southeastern US states that did not expand their Medicaid eligibility, like Alabama, had lower screening rates at publicly funded, low-income clinics and higher mortality-to-incidence ratios, which suggests lower chances of survival, for cervical cancer.[50]
Racial disparities are stark. Of the 4,115 people who died of cervical cancer in the US in 2014, 796 were Black.[51] This means almost one in five women who died from cervical cancer were Black, a troubling figure considering that African American persons make up about 15 percent of the US population; the number of Black women dying from cervical cancer is 1.29 times higher than expected based on their share of the general population.[52]
Black Alabamians are twice as likely to live in poverty as white Alabamians.[53] But racial disparities in cervical cancer deaths are not reducible to disparate income levels. Studies have found that controlling for socioeconomic status reduces the higher cervical cancer mortality risk for Black women, but it does not erase it entirely.[54] Even among women with similar stages of the disease, Black women are less likely to receive treatment due to loss of follow-up, therapeutic delays, and differences in treatment.[55] States that did not expand Medicaid, like Alabama, have higher proportions of African American people, people of low socioeconomic status, and uninsured people, than those that did expand their Medicaid programs.[56] As expansion states have had sharper drops in their uninsured populations, existing cancer outcome differences between states that did and did not expand their Medicaid programs are likely to widen.[57]
Generally, more cervical cancer screenings mean less cervical cancer deaths. The fact that Black women obtain screenings at slightly higher rates than white women contradicts those findings.[58] Rather, experts agree that the lower relative survival and higher mortality rates for Black women are likely due to later-stage diagnosis, treatment differences, and comorbid conditions.[59] The later-stage diagnosis can be explained in turn by failure to follow up from abnormal screenings and diagnostic delays, that is, delays between an abnormal result and cervical cancer diagnosis.[60] Studies have found that race, along with a host of other factors like age, health insurance status, understanding of HPV, and psychological distress, is correlated with poor follow-up after abnormal Pap tests.[61]
Treatment differences after a cervical cancer diagnosis also play a part in outcome disparities. Multiple studies have found differences in the receipt of appropriate treatment along racial and ethnic lines, even after accounting for staging.[62] Ultimately, cervical cancer treatment is complex, even for insured women, and options can include surgery, radiation, chemotherapy, or some mixture of them all.[63] If the process is difficult for those with insurance, it is even more complicated for poor, uninsured women given data showing that socioeconomic status and health insurance coverage are influential factors in both diagnostic and therapeutic delays, or delays between diagnosis and treatment.[64]
Cervical cancer is one of only three cancer locations for which five-year survival rates in the US have not been improving, and like incidence and mortality, there are persistent racial disparities in cervical cancer survival.[65] What’s worse, Black women appear to be losing ground where their chance of surviving more than five years after a cervical cancer diagnosis is concerned.[66] Poverty is certainly a key factor. But neither differential screening rates nor differences in socioeconomic status completely explain away racial disparities in health outcomes.
Alabama and the US South Have High Rates of Cervical Cancer and Poor Indicators of Health
The US South is a racially and ethnically diverse area containing over one-third of the nation’s population.[67] People who live in the US South are more likely than the rest of the nation to be uninsured, live in poverty, have poor health, and have worse health outcomes.[68] Southern women, in particular, have higher rates of smoking, cervical cancer death, heart disease, diabetes, and HIV, than women in other regions of the US.[69]
Human Rights Watch focused on Alabama in some respects because it is representative, and in other important ones, it is anomalous. On one hand, the state’s health environment is typical of other Southern states. It has struggled with high rates of poverty, hospital closures, and poor health indicators. On the other hand, it is unique in having paradoxically both high cervical cancer screening rates and the highest cervical cancer mortality in the nation.
The state ranked 47th in the nation in terms of overall health, losing only to three other Southern states—Arkansas, Louisiana, and Mississippi—for the distinction of worst health in the US.[70] It ranks even lower in the health and wellbeing of women.[71] It is the sixth poorest state in the US, with Black and Hispanic residents falling below the poverty line at over twice the rate of white residents.[72] The unemployment rate in Alabama is significantly higher than the national average and it has the fifth lowest median household income in the nation.[73]
High poverty, unemployment, and rates of uninsured adults combined with an overburdened social safety net, scant public transportation, and gynecological shortages, create a treacherous health care environment in Alabama. According to the most recent CDC data available, in 2015, Alabama was tied with Kentucky for the third highest incidence and had the single highest death rate for cervical cancer in the nation.[74] About 235 Alabamian women are diagnosed with, and over 100 die from, the largely preventable disease each year.[75] Moreover, things appear to be getting worse. The rate of cervical cancer cases and deaths increased 18.2 percent and 34.5 percent respectively between 2010 and 2014.[76]
Cervical cancer is a disease of poverty, but also exclusion. Systemic racial inequality in health has made the situation worse for some poor women. While race-based differences in incidence have steadily narrowed in Alabama since 1999, racial disparities in mortality have stayed relatively constant and remain well above the national average.[77] According to Alabama’s most recently reported numbers, Black women die at almost double the rate of white women from cervical cancer: 5.2 compared to 2.7 per 100,000 women.[78] Moreover, research indicates that because cervical cancer rates have been historically miscalculated, those numbers likely underestimate true racial disparities in mortality rates.[79] If Alabama reflects nationwide trends, the corrected rate would likely show that Black women die at over twice the rate of white women from a preventable and curable disease.[80]
In Alabama, the percentage of Black women being screened for cervical cancer is more than 10 percent higher than the number of white women, and well above the national average.[81] This means that, on average, missed screenings cannot explain the disparate mortality rates. Follow-up care and treatment are key. Ensuring that women can get past the abnormal Pap tests to diagnosis and treatment is an integral part of addressing racial disparities in mortality rates.[82]
Alabama’s Black Belt Is a Hub of Socioeconomic Deprivation and Poor Physical Health
Local experts identified the Black Belt as an area where women, and particularly Black women, face unique challenges in accessing reproductive health care. The Black Belt is a center of rural Black America.[83] Originally, the term “Black Belt” referred to the naturally rich, dark soil in a strip from central Alabama to Mississippi. After the turn of the 20th century, the Black Belt moniker came to designate the counties with a majority Black population.[84]
Alabama has 67 counties and opportunities for health care vary significantly depending on where one lives.[85] Because of data limitations, county-level rates of cervical cancer incidence and mortality are unavailable in some cases and unintentionally misleading in others.[86] But there are predictors for areas where cervical cancer deaths are more likely: populations with high poverty rates, low education rates, no insurance or public insurance, and lack of access to a regular provider. These factors coincide in the Alabama Black Belt.[87]
Alabama’s Constitution was adopted in 1901, and the convention’s president, John B. Knox, asserted that its aim was to “establish white supremacy in this state.”[88] The state constitution, which still governs today, diminished the electoral influence and educational opportunities of the Black Belt’s majority African American population and continues to mandate school segregation (although this provision has long been invalidated by federal law).[89] Geographic isolation and de jure turned de facto segregation have helped shape health and wellness in the Alabama Black Belt. The area has poor health, poor access to health care services, and poor education opportunities, along with high rates of poverty, unemployment, and uninsured adults. It therefore has the conditions in which one would expect more preventable cervical cancer deaths to occur.
The Black Belt is a hub of physical, social, and economic deprivation in an already poor state. Nine of the ten counties with the highest poverty and lowest median income in Alabama are in the traditional Black Belt region.[90] For context, consider that in the US about 14 percent of the population is living in poverty. In Alabama, that number is 17.2 percent, or a little more than one in every six people. In the Black Belt, the poverty rates range from a high of 35.4 percent in Dallas County to a low of 18.8 percent in Montgomery. In most Black Belt Counties, one out of every three or four residents are living in poverty.[91] Moreover, eight out of the ten worst Alabama counties for overall health outcomes are in the Black Belt and it has some of the highest rates of unemployment, adult smoking, new chlamydia cases, and HIV prevalence.[92]
This is a substantive racial equality issue. Alabama is a state of 4.75 million people. A little over half are female and a little over a quarter—26.8 percent—identify as Black or African American. In the Black Belt, on the other hand, all counties except one have higher African American populations than the state average, and in over half, the majority of residents are Black.[93] Macon, Greene, Lowndes, Sumter, and Wilcox counties, moreover, are over 70 percent African American.[94]
A legacy of deep community empowerment and political engagement exists aimed at overcoming a history of abuse and contemporary manifestations of racial injustice. The Alabama Black Belt is home to places that stood in the center of the civil rights movement, such as Selma, Tuskegee, Lowndes, Dallas, Montgomery, and Marion.[95] Activists and community members continue to campaign against systemic harms like voter disempowerment,[96] unequal education opportunities,[97] and environmental injustice.[98] Just this year the Equal Justice Initiative opened the National Memorial for Peace and Justice in Montgomery. It is the first of its kind, dedicated to the victims of racial terror and white supremacy.[99]
Human Rights Watch spoke to over a dozen community groups and organizations that are working in their own way to build health and wellness in the Alabama Black Belt.[100] But, as Felicia Lucky from the Black Belt Community Foundation explained, the state had a hand in creating systems of racial inequity and needs to act with intentionality to undo their effect: “These systems have been created to take power from people, to make them feel powerless.…It didn’t happen by happenstance. It was intentional that those things happened, and to undo it, we have to have the same intentionality.”[101]
|
Past Racist Policies and Practices Impact Health in the Black Belt The Tuskegee syphilis study and the Relf case are two examples of government-sponsored medical exploitation and mistreatment of poor Black patients in the Alabama Black Belt. Both were programmatic abuses that originated in Macon County and show how past state and federal policies supporting white supremacy can fracture community trust in the medical profession. From 1932 through 1972, the US Public Health Service (USPHS), in coordination with the Tuskegee Institute, enrolled hundreds of poor Black Macon county sharecroppers in a study on the natural history and progression of syphilis.[102] Officials never told participants they had syphilis nor were they treated, even after the discovery of a cure for the disease and the establishment of USPHS syphilis treatment centers. The US government gave participants reparations in 1974 in the form of a class action settlement and lifetime medical benefits.[103] Nevertheless, multiple health care providers told Human Rights Watch that the memory of Tuskegee continues to fuel mistrust of the health care system today, especially for older patients. “We have a lot of elderly patients, and with them being elderly, they have heard stories about certain programs, certain treatments like the Tuskegee syphilis study…. I don’t think we’ve had many patients [from the study], but they’ve heard stories about it. You know, from granddaddy. And it’s still in the back of their mind. There’s a trust factor.”[104] The syphilis study is one example of how structural racism has manifested in medical practices.[105] The year after the Tuskegee syphilis study ended, the involuntary sterilization of two African American sisters, also from Macon county, came to light. The ensuing court case revealed sterilization abuse across the nation that spanned decades. Doctors and nurses threatened to terminate welfare benefits belonging to women—many of whom were Black or with intellectual disabilities—if they did not agree to be sterilized, leading to the federally-funded sterilization of an estimated 100,000 to 150,000 poor people annually without informed consent safeguards.[106]
The case incited a national conversation about racism, eugenics, and reproductive freedom in US family planning clinics.[107] “What was going on through the ‘60s and early ‘70s was simply sterilizations, particularly in the South, of Black kids, Black women in order to avoid reproduction of more Black people. It was basically a eugenics program,” Joseph Levin, attorney for the Relfs from the Southern Poverty Law Center told Human Rights Watch.[108] The egregious, widespread injustice of the state-sponsored interference with Black women’s autonomous reproductive decision making occurred unchallenged for decades. The Relf case led to the federal requirement that physicians obtain full, informed consent for sterilization procedures.[109] Nevertheless, more than 40 years after the Relf case was dismissed, women interviewed by Human Rights Watch still experienced uncertainty about why they received hysterectomies. Blythe S., 62, of Greene county, had a hysterectomy in 2007 after having heavy bleeding during her period, but the doctor never explained why. “I dunno,” Blythe said. “I dunno what they did to me. I really don’t.”[110] Cynthia H., 55, of Greene county, is also not sure why she needed a hysterectomy. She went to the hospital for a follow-up procedure after an abnormal Pap smear and was told that she would need a “scraping,” likely an excisional procedure to remove precancerous cervical cells, or a hysterectomy. “It [the scraping] didn’t work I don’t think because he told me I needed a hysterectomy.”[111] These cases inform women’s own experiences of callous reproductive health care. A woman who had a hysterectomy after a painful colposcopy and cryotherapy, for example, told Human Rights Watch, “I feel like he [the gynecologist] just looked at me as a Black woman and just slaughtered me.”[112] She should continue to have cervical cancer screenings, but refuses: “I just don’t want them touching me…”[113] Tuskegee and Relf are indispensable historical and social context for understanding why it is particularly concerning to hear a gynecologist from Selma raise concerns that untrained doctors come to rural areas to effectively “practice” on women or that some patients remain concerned that providers recommend hysterectomies inappropriately.[114] “Doctors use hysterectomies as a form of birth control,” one woman said. “They take your uterus; they take your cervix and then they don’t have to bother with you anymore.”[115] |
III. Gaps in Alabama’s Social Safety Net Contribute to Cervical Cancer Mortality
Alabama’s high cervical cancer mortality rate exposes failures in the state’s bare-bones public health care coverage. The state does not guarantee access to consistent coverage for reproductive health care and the multiple publicly funded programs through which women can access cervical cancer related care each have flaws and limitations.
A handful of narrowly focused, non-comprehensive programs help to extend health care coverage to select populations or for select services. But Alabama’s approach to public health care still leads to fluctuating insurance eligibility. Moreover, potentially prohibitive costs for colposcopies and cervical cancer treatment means women who need more advanced care are especially vulnerable. Ultimately, poor and low-income women are at risk of falling through the holes in Alabama’s patchwork public health system.
This section will describe health care coverage in Alabama and how state and federal government policies threaten to further damage it. It also details the impact these policies have had on women facing immense challenges because of inconsistent health care coverage.
Underserved Women at Risk: Impact of Inconsistent Access to Reproductive Health Care Services
Cervical cancer mortality persists despite multiple programs providing coverage for prevention or treatment. Alabama could improve health care coverage by expanding its Medicaid program, but is instead taking steps that would further destabilize coverage in the state. Alabama programs and federal regulations do not adequately address the unique challenges that insurance coverage for colposcopy and diagnostic testing presents to Alabama women. The federal government has also taken steps that undermine the Patient Protection and Affordable Care Act, which will decrease insurance coverage in Alabama.
No Public System Ensures Consistent Coverage for Prevention, Treatment of Cervical Cancer
Alabama uses state and federal programs to string together reproductive health care services for poor and low-income women. Different programs have different, and sometimes fluctuating, eligibility standards and cover different services. This means that an uninsured woman could get her screening through one program, her colposcopy and diagnostic services through another, and her cervical cancer treatment through a third, assuming she meets the eligibility criteria for all of them.
The state Medicaid program provides one explanation for this. Very few abled-bodied, non-pregnant adults in Alabama are eligible for full Medicaid coverage, which would enable low-income and disabled people to access health care, such as preventive and emergency services, with limited or no out-of-pocket costs.[116] Medicaid is jointly funded by the state and federal governments. The federal government sets the minimum requirements for eligibility and benefits while states can shape how the program functions, that is, by defining the eligible population, covered services, and methods for paying participating doctors and hospitals.[117] Medicaid is an essential part of the US health care system, covering about 1 in 5 people and financing nearly 20 percent of personal health care spending.[118]
Right now, Alabama is tied with Texas for the lowest Medicaid eligibility levels in the nation.[119] An able-bodied adult who is not a caregiver or pregnant is ineligible for full Medicaid coverage, no matter how poor the individual is. For a caretaker to be eligible, they must be living in extreme poverty, making less than 18 percent of the federal poverty line or $2,196 annually.[120]
Special groups qualify for incomplete or temporary Medicaid coverage.[121] Pregnant women above the caretaker income threshold can receive maternity coverage, including full Medicaid benefits, if their income is below 146 percent of the federal poverty line, or about $17,724 per year for a one-person household.[122] But that coverage ends three months after the woman gives birth. Non-sterilized women ages 19 to 55 at the same income level qualify for the state’s family planning program, Plan First. The county public health departments also offer free or low-cost family planning services. Altogether, able-bodied adults, including those on family planning, make up less than 20 percent of the people on Alabama Medicaid in part due to the program’s severe income restrictions.[123]
In Alabama, “family planning services” includes things such as birth control, sexually transmitted infection (STI) testing and Pap smears, but not follow-up care from abnormal screenings.[124] To help cover this gap, the joint federal and state Alabama Breast and Cervical Cancer Early Detection Program aims to increase access to breast and cervical cancer services for uninsured or underinsured women.[125] It covers cervical cancer screenings, colposcopies, and diagnostic testing. [126] The program extends coverage for eligible women even if they were screened by another program, like publicly funded family planning.[127] In practice, however, the ABCCEDP faces funding and outreach limitations.
Despite the public options for prevention and screening, before 2010 there was no coverage for the treatment when someone was diagnosed with cervical cancer. In 2010, the Breast and Cervical Cancer Treatment Program (BCCTP) addressed that significant flaw, extending full Medicaid benefits to uninsured women under 65 with breast or cervical cancer.
The consequence of providing different programs with different services and different eligibility is delay, confusion, and forgotten women. One study found that after the BCCTP was established, treatment delays worsened in part because of obstacles imposed by the Medicaid enrollment process.[128] The harm was especially acute for Black women, whose chance of meeting the standard for the initiation of cancer treatment decreased by almost 10 percent, but the reason for this disparate impact is not clear from the study.[129]
Inexplicably, BCCTP Medicaid benefits terminate once the person is determined to be cancer-free, leaving uninsured cancer survivors without coverage for necessary maintenance tests and treatment to ensure that the cancer does not recur.
The US has a publicly-funded health insurance program called Medicare for adults over 65 years old. Medicare Part A is generally premium-free and covers hospital and nursing facility care.[130] Medicare Part B, which is more comprehensive and covers medically necessary and preventive services, does require a monthly premium.[131] For those under 65, health insurance is often contingent on employment status; over half of adults under 65 have health insurance through their employer.[132] Those who do not—whether because their employer does not offer health insurance, they are employed part-time, or they are experiencing unemployment—have to purchase insurance themselves, leaving them at higher risk of being uninsured.[133]
For the uninsured and underinsured, the public health care system is crucial. Rather than taking a comprehensive approach to public health care, state and federal programs are created or shift as gaps in treatment become clear, tacking women’s health care services onto the Alabama social safety net. Mani M., a 40-year-old cervical cancer survivor from Perry county said, “It’s fortunate that we have the community partnerships that we have. But when it comes to women…. Well, I think the health care system was originally built for men.”[134]
Resources Exist to Expand Medicaid, Instead Alabama Wants to Make Medicaid Stingier
The state legislature or governor could act to improve coverage for poor and low-income people with the help of federal government funding, but they have chosen not to. Instead, Governor Kay Ivey has requested special permission to make Alabama’s Medicaid eligibility even more restrictive by imposing counterproductive work requirements, undermining efforts to increase access to life-saving cervical cancer care.[135]
Under the Patient Protection and Affordable Care Act (ACA), states can use federal funds to expand their Medicaid programs and cover more people.[136] The formula established by the ACA effectively means that residents below 138 percent of the federal poverty level—whether or not they have children, are pregnant, or are disabled—would be eligible for Medicaid coverage in the states that expand coverage. The federal government paid 100 percent of expansion costs for the first 3 years, beginning in 2014, and will phase down to 90 percent by 2020.[137]
Alabama struggles to fund its bare-bones Medicaid program. A one-time oil spill settlement made up for recent budgetary shortfalls, but that money has run out. Carryover from the 2017 budget, attributable to lower drug costs and decreased Medicaid enrollment, helped offset the need to increase state funding, but it is not clear that the savings are sustainable.[138]
In 2015, then-Governor Robert Bentley created the Alabama Health Care Improvement Task Force in response to concerns about the “serious shortage” of physicians in rural Alabama.[139] The task force unequivocally recommended that the state expand Medicaid.[140] Yet neither current Governor Kay Ivey nor the Alabama legislature have acted to expand Medicaid coverage to the estimated 153,000 people who could benefit, most of whom have no other realistic access to health insurance coverage.[141]
Medicaid expansion has been shown not only to increase access to comprehensive health services, but to reduce poverty, a primary driver of cervical cancer risk in the US.[142] It could help stabilize and support a buckling healthcare system, decrease the risk of rural hospital closures, and create new opportunities for employment. By not expanding its Medicaid program, Alabama lost $14.4 billion of federal Medicaid funding and is leaving $4.9 billion unclaimed over the next decade.[143]
Unlike Alabama, states that have expanded their Medicaid programs have seen increased access to care and more significant reductions in health care access disparities compared to states that have not expanded their Medicaid programs.[144] The ACA has especially benefited vulnerable populations, with the largest coverage gains since 2012 made by people of color, poor and low-income individuals, and people without a college degree.[145]
People living in rural areas have benefited most of all from states’ decision to expand Medicaid. Rural areas in states that expanded have seen increased Medicaid coverage and reduced uninsured rates. In fact, non-elderly residents in states that did not expand their Medicaid programs are nearly twice as likely to be uninsured compared to those in rural areas in states that did.[146] Moreover, rural hospitals in states that expanded Medicaid are significantly less likely to close than those in states that did not do so.[147]
Rather than securing better coverage for Alabama residents, the state is going in the opposite direction.
The Ivey administration submitted a proposal to the Department of Health and Human Services (HHS) on July 31, 2018 to add work requirements to Alabama Medicaid.[148] Under the proposal, caretakers would have to work at least 35 hours, or 20 hours if they have children under 6 years of age, per week to be eligible for Medicaid. In a particularly cruel catch 22, any caretaker who meets the work requirement—working, for example, at least 20 hours per week at minimum wage—would exceed the Medicaid income limitations and be ineligible for coverage, unless they had eight or more dependents.[149] An estimated 8,700 of the poorest Alabamians would lose Medicaid coverage in the first year, with women, African American persons, and families in rural communities taking the hardest hit.[150]
The Ivey administration’s proposal is short on implementation details. Advocates fear that the process of verifying whether applicants are complying with the work requirements will drive up administrative costs and result in people losing coverage not because they were not working, but because they did not file the necessary paperwork.[151]
Alabama’s Safety Net Does Not Adequately Cover Colposcopies and Other Follow-up Care
Regular screenings are essential to preventive care but, by themselves, are not enough to prevent cervical cancer deaths. A systematic review of follow-up care after abnormal cervical, breast, and colon cancer screenings showed that about one in four screened women did not receive timely and appropriate follow-up care.[152] In Alabama, the ABCCEDP is the only public program specifically structured to bridge the devastating gap in the Alabama health care safety net: coverage for colposcopies and diagnostic tests for uninsured and underinsured women. However, budgetary restrictions limit the effectiveness of the program.
Women with private insurance, Medicaid, or access to the ABCCEDP or the county health department should be able to obtain a cervical cancer screening without any out-of-pocket cost.[153] For women without those options, a Pap test could range from $20 to $75 and an HPV test could cost $80 or more depending on laboratory fees—figures that are unaffordable for some women.[154]
Colposcopies and biopsies are significantly more. If a screening reveals an abnormal result, the cost for the necessary follow-up care can be prohibitive for the insured and uninsured alike. Despite being necessary aspects of cervical cancer prevention, colposcopies and biopsies are not covered as preventives service under the ACA’s essential benefit mandate or as family planning services under the Alabama Medicaid Administrative code.[155] The exclusion of colposcopies and diagnostic testing means those services are less affordable and accessible, even for insured women.[156]
Screenings are entirely ineffective at preventing the development of cervical cancer if women do not receive follow-up services. Dr. Warner Huh, the director of the only low-income colposcopy clinic in Alabama, explained:
Even though screening is provided for free to women who are insured, the diagnostic procedure is not. So yeah, your $35 Pap is covered but your $1,000 colposcopy and biopsy isn't. Well, that doesn't help anybody, right? So, if you're screened and have an abnormal test, that's only one piece of the pie.... Yeah, get screened. But will we have a way for you to get treated and managed when there's an abnormal screening test?[157]
The ABCCEDP is a key avenue in Alabama for coverage of colposcopies and other follow-up services. Program staff have shifted eligibility standards to serve women left out by the state’s family planning program: women between the ages of 30 and 39 with tubal ligations and those covered by Alabama Medicaid’s family planning program who need colposcopies or diagnostic procedure.[158] In the future, program staff hope to extend eligibility to women in their twenties whose follow-up care is similarly not covered by Alabama Medicaid’s family planning program.[159]
Severe financial constraints limit the program’s effectiveness despite efforts at increasing its reach. The legislature appropriates some funds for the program but not enough to meet the state’s obligation to contribute $1 for every $3 provided by the federal government. Instead, the program makes its match through providers’ donated work and time.[160] The Medicare rate is less than providers’ usual and customary fee. Therefore, “they are taking a loss when agreeing to see women at the Medicare rate," as Nancy Wright, the director of the Alabama Department of Public Health division that heads the ABCCEDP, said.[161] The program counts the amount that providers are underpaid as though it is a state contribution for the purposes of making the $1 match.[162]
State appropriations for the ABCCEDP have been relatively stagnant over the past decade.[163] The 2018 budget includes the first funding increase in years: from $383,500 to $500,000.[164] “It’s gone up and down. Most of the time, if you look over a 10-year period, it stays the same,” Wright explained.[165]
Federal funding has also recently shifted. It took a devastating hit in 2017, when the Department of Health and Human Services cut the National Breast and Cervical Cancer Early Detection program (BCCEDP)—which is the source of the matching funds—by $40.8 million or about 15 percent of its total budget.[166]
Additionally, the CDC has changed its approach to state BCCEDP grants. The grant process is essentially pushing the ABCCEDP from a need-based approach that prioritized direct services to the uninsured and toward a multi-level approach that includes other priorities, such as fostering environmental, workplace, and health system changes, in addition to the provision of direct services.[167] Because the ABCCEDP must implement the new and old components equally, less money is available for direct services. “You only have so much and when you divert it to do other things that means there will be less direct services for women who have no insurance,” Wright explained.[168]
The goal of the new approach, according to Wright, is to create systemic changes that will improve health care access for insured and uninsured women alike.[169] However, both the budget cuts and new grant approach are predicated on insurance gains made through the ACA marketplace and the option to expand Medicaid coverage to low-income people, which Alabama has not done.[170] At the same time, health care coverage improvements risk regression under new federal actions.
Wright agrees with the premise of the new grant focus. However, she reported fearing the new approach could lead to increased demands that the state cannot meet, especially with a reduced direct services budget:
I can tell you that I was very resistant because it has always been from the beginning that our role was to help directly provide services to women who are in need. So, I was very resistant to working with the system or workplace or do outreach, because how do you do more outreach and bring more people in if you can’t pay for the direct services? [171]
Minimal state and federal funding means that most woman who are ABCCEDP eligible fall through the cracks. An estimated 70,000 Alabamian women, or 82 percent of those eligible, are not accessing the program and marketing is tightly restricted.[172] Program staff members cannot do outreach to all eligible women because doing so risks bankrupting the program.
Our money matches our enrollment. If we get x amount of money, we can see maybe 15,000 women. If we advertised, we would exceed and get 17,000 or 18,000 women and we wouldn't have the funds to pay that. So, marketing is very challenging, very restrictive…[173]
To run the underfunded program, ABCCEDP staff adjust eligibility requirements to cut down on the number of women accessing services when the budget is tight. This has led to significant inconsistency in the eligibility guidelines over time.
Over the past 12 years we’ve been together, we’ve increased eligibility and we’ve decreased eligibility. We’ve increased and decreased, always trying to make minimal, minimal changes because you can’t just change it because doctors don’t respond to change that fast and there’s appointments ahead of time.[174]
An ABCCEDP official told Human Rights Watch that not all eligible women are receiving colposcopy coverage through the program, not because the program is unavailable to them but because providers are not enrolling them in ABCCEDP. Instead many women seek other avenues for care, such as sliding scale clinics. Those services may require unaffordable co-pays or high transportation costs to reach that may make these services inaccessible to women living in poverty.[175]
Usually the primary health providers, the county health departments who are referring, they know about the patients. So, if they knew that the patient doesn’t have any money or they cannot refer, then they come to us. Most of the time, I think if the patient has some avenues or something is covered, usually it goes through sliding scale.[176]
Human Rights Watch understands this means that some otherwise-eligible women miss the opportunity to enroll for full ABCCEDP coverage for colposcopies and are instead referred to a reduced-cost service provider. This does not mean they are barred from enrollment. As ABCCEDP officials have clarified to Human Rights Watch, “[e]ven if the patient was not enrolled to begin with, [the program] will step in and provide coverage.”[176.5]
Dr. Stevens, one of the only obstetrician gynecologists in the central portion of the Alabama Black Belt, told Human Rights Watch that the cost of the colposcopy and biopsy is enough to keep women from care even when it is reduced:
There are a lot of people who the health department will make the appointment for the patient, and they won't show up. It's understandable if they don't have any insurance and they're afraid that they'll have to pay because, you know, a lot of people will charge a decent amount of money. We charge only $150 to do a colposcopy.[177]
The financial constraints that his patients are under have impacted the way he treats women. He will avoid doing a biopsy along with the colposcopy unless it is strictly necessary because his patients often cannot afford the laboratory fees: “And I don't do any biopsies hardly ever.... They're probably $300 per biopsy.”[178]
Reduced-fee procedures are available at the UAB Colposcopy Clinic, which charges $60 for a colposcopy—or more for additional procedures—but can waive or reduce the fee. However, for this option, travel and limited availability replaces cost as a barrier. Some women drive three or four hours both ways to attend an appointment.[179] The clinic is only open for colposcopies on Friday mornings, creating additional burdens for women who are not able to take time off work or find child care.[180] These challenges contribute to the clinic’s low follow-up rate, which is consistently less than 50 percent.[181]
Actions by the US Government Decrease Insurance Coverage in Alabama
Federal actions threaten to undo the health care coverage improvements that have been made. Congress repealed the individual mandate of the ACA, which had created a tax for people who do not have health insurance. The repeal raised fears that younger, healthier people will not obtain insurance, lowering coverage rates and increasing health insurance prices for those who do.[182]
Hours into his presidency, US President Donald Trump signed an executive order to “minimize the economic burden of the Patient Protection and Affordable Care Act” pending its “prompt repeal.”[183] The order led the Internal Revenue Service to change its practices and process tax returns even if they do not meet the ACA’s required minimum coverage.[184] President Trump also signed an order allowing new, unregulated insurance packages that risk undermining the long-term viability of key innovations in the law, potentially making coverage too expensive for people with greater health care needs. Furthermore, President Trump threatened to halt federal support for health care subsidies, a critical source of funds that help people under 250 percent of the federal poverty level afford to buy health care on the ACA marketplace, a state-facilitated or federally-facilitated place where uninsured people can learn about, compare, and purchase health insurance plans.[185]
The Trump administration took aim at public outreach and information about ACA enrollment. HHS cut advertising for open enrollment by 90 percent, reduced grants for navigators who help people sign up for health insurance through the ACA marketplace, by about 40 percent, and cut the open enrollment period in half.[186] The administration also issued regulations that could weaken the requirement that health plans include certain essential health benefits such as preventive services, prescription drugs, and maternity and newborn services.[187]
A recently released nationwide analysis predicted that such federal actions will have a devastating effect on insurance premiums for health plans. Premiums are likely to increase between 36 and 94 percent around the country by 2021 due in part to the recent changes on the federal level.[188] Specifically, health insurance enrollment through Alabama’s marketplace decreased 5 percent in 2017 and, the analysis predicts, will experience a “catastrophic” increase in premiums of up to 90 percent by 2021.[189]
Impact of a Weak Public Health Safety Net on Women’s Use of Preventive Cervical Cancer Care
One consequence of the state and federal government’s patchwork approach to public healthcare is that residents have fluctuating access to coverage and services. This section presents the experiences women relayed to Human Rights Watch about how the structure of the Alabama public health care system has failed them in moments of crisis and how being uninsured changes their health care choices.[190] The Alabama legislature could ensure that women living at or near the poverty line have consistent coverage by expanding its Medicaid program under the ACA, but has not done so.
The women interviewed described how major life events like pregnancy, spousal injuries, or job loss led to changes in their insurance status. Those changes, in turn, affected their willingness to seek reproductive health care. Even when low cost or free public services were technically available, women said the loss of health care coverage still impacted their decision making. One woman described her happiness when enrolling in the Alabama Medicaid maternity coverage program.[191] She was uninsured before her pregnancy and much prefers her obstetrician gynecologist to the public health department. However, that coverage will end three months after she gives birth.
Others described how their insurance coverage was dependent on their employment status.[192] Bouts of unemployment meant bouts without health care. Blythe S., 62, of Greene county, went through a number of jobs after the plant where she worked for a decade closed.[193] “I started off working for the sewing plant for 10 years. And then after that closed down, I went to North Port, packing car parts and stuff like that. And then on and on and on.” Most of the time she had insurance when she was employed, but would sometimes lose coverage when her employment status changed.[194]
Residents of the Alabama Black Belt experience some of the worst unemployment rates in the state. Wilcox county, for example, had an unemployment rate of 11.4 percent in 2017, dwarfing the national and state averages of 4.4 percent.[195] Greene county, where Blythe and Hazel B., 47, live, has the fifth highest unemployment rate in the state at 7.7 percent.
Hazel lost her health insurance in 2012 after she was laid off from her job.[196] She did not regain coverage until 2015 when she enrolled in Medicaid because of a disability.[197] As a survivor of breast cancer and what she described as a horribly botched hysterectomy, she did her best to consistently access health care. “I was getting Pap smears ever since I had health insurance, when I was working,” she told Human Rights Watch. But after becoming uninsured, she avoided any non-emergency contact with the health care system: “If I didn’t have to go the doctor, I didn’t go.”[198]
The ultimate danger of inconsistent and fluctuating health care coverage is that preventive screenings and early warning signs will be missed during periods without insurance.
Darcy C. and Kira D. both battled endometrial cancer, which develops in the lining of the uterus.[199] Both women said their loss of health insurance was a key factor in their failure to obtain Pap tests prior to their cancer diagnoses. There is no routine screening test for endometrial cancer.[200] However, the Pap test can sometimes find cellular changes that could indicate precancerous or cancerous endometrial cells.[201] When such atypical cells are found, an endometrial biopsy can be used to diagnose cancer.[202]
Darcy C., 57, of Choctaw county, had insurance until 2001 when her husband, the sole provider in their family, was incapacitated after a tree fell on him.[203] In 2015, she was enrolled in Medicaid because of a disability. The same year she found out she had stage II endometrial cancer. Between 2001 and 2015, she did not go to the doctor or have a Pap test. She believes that is part of the reason why her cancer was not detected earlier.
I believe I had it [cancer] but I didn't have health insurance so I didn't go. That is really why I did not go, because I would bleed sometimes, like, a month and stop for 2 or 3 days and then I would bleed a whole 'nother month.… And I know with me not having health insurance, and they want to send me to another hospital, I didn't have the funds to go.[204]
After a total hysterectomy and regular chemotherapy covered by Medicaid, Darcy’s cancer was in remission in late 2015. In May 2017, a mass next to her spine revealed the cancer had returned, which sent her back into treatment.[205]
Kira D., 71, of Greene county, is caring for two young foster children and is living with stage IV endometrial cancer.[206] She lost her health insurance after she retired at 62. She remained uninsured until she became eligible for Medicare in 2012.[207]
Kira had one Pap test at the public health department when she was 62 and after losing health care coverage.[208] The results of the test were abnormal. The repeat test returned a normal result and then, she told Human Rights Watch, she never went back for additional care.[209] She did not see the point of doing so; if she did need additional follow-up, she would not be able to afford it without insurance.
When I retired at 62, I had no insurance … and then from 62ish up until 65, when I got Medicare, then I knew I could go to the doctor and get it [another Pap test]. The health department, they would take me, but I just didn’t go back because I didn’t have no money, no extra money to do anything with. So, I just didn’t go.[210]
Kira’s abnormal screening history suggests that Kira was in the group for whom continued screening is clinically indicated after the age of 65. Kira did not have another Pap test until she noticed vaginal spotting in 2014. That Pap and necessary follow-up tests led to a diagnosis of stage II endometrial cancer.
Some women described periods being uninsured and inadequate screening histories, but did not give a specific reason for why they experienced prolonged periods without cervical cancer screenings.[211] Blythe, who had intermittent health care coverage, sometimes missed cervical cancer screenings: “Sometimes I did, sometimes I didn’t.… I don’t know. Just didn’t go.”[212] Others had similar reactions: “I just didn’t. I just didn’t get there,” or “I just didn’t go.”[213]
These women did not specifically say that a loss of health insurance caused their inadequate screening histories and some were aware that county health departments offer free cervical cancer screenings. Nevertheless, their experiences align with academic literature, which shows that women who do not have access to consistent health care or insurance coverage are less likely to have adequate screening histories.[214]
For some women, other priorities compete with preventive care. Kira told Human Rights Watch that she failed to get cervical cancer screenings for years because it she didn’t have the resources to make it a priority.[215] She explained:
My financial situation wouldn’t allow me, that this was more important than paying for your lights, you water, transportation, you know, your car. Because if I needed assistance, if I needed a doctor, most of the neighbors are gone during the day. And then my family wasn’t close by.… You had to stretch that dollar.”[216]
At times, women will forego preventive care and rely on emergency care only. This can have disastrous effects. Dr. Stevens, an obstetrician gynecologist in Selma, told Human Rights Watch about a 27-year-old woman, who had not had a Pap test in 10 years and went to an emergency room three times because of bleeding after intercourse.[217] Emergency room staff treated her for pelvic inflammatory disease (PID) without conducting a pelvic exam.[218] If they had done one, they would have found what Dr. Stevens found: cervical cancer, at least stage II.
Impact of Inconsistent Use of Health Care Services on Provider Behavior
Inconsistent use of health care services contributes to providers giving cervical cancer screening that do not align with professional guidelines. This section reviews the recommended cervical cancer screening guidelines and presents testimony from women and providers that strongly suggests a pattern of over-screening for cervical cancer. Providers explained that they prefer to over-screen because of concerns that women will not return for appointments. This diverts much needed resources from an already grossly underfunded public health care system. Alabama should investigate the extent and consequences of over-screening. The state should address the issue by adequately funding the ABCCEDP and taking steps to increase screening and follow-up rates.
Cervical Cancer Screening Guidelines Have Changed Significantly in the Past Decade
Routine screenings and timely follow-up procedures matter because early detection matters. Approximately 55 to 60 percent of cervical cancer cases are detected in women who were not screened in accordance with federal guidelines; the chance of survival decreases precipitously with later-stage diagnoses.[219] Yet from 2000 to 2015, the overall trend for cervical cancer screening in the US has declined, with the lowest rates among the uninsured and those who lack a usual source of health care.[220] Women who are uninsured, low-income, and live in states that did not expand Medicaid under the ACA report significantly lower odds of receiving adequate cancer screenings.[221]
The recommended screening frequency for cervical cancer has shifted relatively frequently in the US. Major updates to guidelines occurred in 2006 and 2009.[222]
In 2012, the major professional organizations coalesced around consensus guidelines: rejecting annual screening and recommending screening in three- or five-year intervals.[223] The United States Preventive Task Force, an independent panel of private-sector medical experts, funded and appointed by HHS, that makes recommendations on preventive services, followed their lead. Its recommendations are important, impacting what services some federal programs, such as Medicaid and Medicare, and private health insurance plans must cover.[224]
The frequently shifting guidelines have created some difficulties. Experts suggest that women and medical providers have not always been willing or able to keep up with cervical cancer screening guideline changes, and some are still struggling to comply with the 2012 screening guidelines.[225] Nevertheless since 2012, there have been more developments and the USPSTF updated its recommendations again in August 2018. The current recommendations are:
· No cervical cancer screening before the age of 21;
· Women ages 21 to 29 should receive a Pap test once every three years. They should not receive an HPV test because of the high prevalence of self-clearing HPV in that population;
· Women ages 30 to 65 should receive co-testing – Pap and HPV testing – every five years, a Pap test every three years, or high-risk HPV testing alone every five years;
· Women older than 65 should not receive cervical cancer screening unless they have unknown or inadequate screening history or are at high risk of cervical cancer.[226]
In this update, the USPSTF included more cervical cancer screening strategies, effectively expanding the types of screening that many health plans must cover without co-pay.
Over-screening When Reproductive Health Care Access Is Inconsistent
The uncertainty of insurance coverage in Alabama is one factor that negatively impacts the health-seeking behavior of women in the state. Human Rights Watch found that it also affects provider behavior. Women often do not know the appropriate screening intervals. A vast majority of the women Human Rights Watch interviewed expressed a belief that it was important to receive annual Pap tests, regardless of whether they actually received them.
Annual Pap tests are a recognized form of over-screening, but providers still order them. Dr. Warner Huh, Division Director of Gynecologic Oncology at the UAB and an expert in cervical cancer care, explained that providers’ uncertainty about whether women will come back for additional screening encourages over-screening. In a sense, providers want to capture women while they can.
There's always the tendency to over-screen and over-treat. That's been always sort of the motto. You're better off over-screening and over-treating than doing it the other way around. And so, if there's a judgement call made by the health departments, they favor having the patient be seen too much rather than too less.[227]
Younger women and providers told Human Rights Watch that county health departments condition the receipt of birth control on having a Pap test, leading to frequent screening.[228] Vanessa T., 20, of Sumter county, has already received three Pap tests from her county health department. “My first one I had to get before I got on birth control. And after that one, they made sure I got one every year.”[229] According to guidelines, Vanessa should not start receiving Pap tests for another year.
Darlene W., 22, of Perry county, said that when she was 19 or 20 years old, the health department told her that if she wanted birth control she would have to have a Pap test.[230] Her tests were never abnormal, never required rescreening, and yet Darlene described receiving one or two Pap tests per years and, in total, three or four.[231]
For both women, the county health department began screenings earlier, and performed them more frequently, than indicated by federal guidelines.
This issue is not confined to the public health department. Dr. Stevens said that he, too, errs towards over-screening. “We probably do what I would consider sometimes unnecessary pap smears just because we're afraid that person might not be back in any time soon to get a Pap.”
Implementation of the guidelines must be paired with patient education. If women believe they should receive annual screenings, they may feel mistreated by providers who screen them less frequently. One woman, 62, described a heated conversation with her doctor when he told her that she did not need an annual Pap test anymore:
I asked him while he was talking, “Now hold up! You tryin’ to tell me just because I’m old I don’t need to take them?”.... I just want to understand it because you ain’t going to tell me I can’t come back and get that Pap smear.[232]
Under-screening of Women Over 65 Puts Some at Higher Risk of Cervical Cancer Death
Nearly all the women with whom Human Rights Watch spoke described providers recommending cervical cancer screenings at regular intervals—some even more frequently than indicated by federal guidelines—with one notable exception: older women.
The failure to recommend screening appropriately for older women is not surprising. According to Claudia Hardy, an expert in minority health who has more than 15 years of experience with cervical cancer related community outreach in Alabama, screenings have traditionally been linked to maternal health, which puts older women at risk. Hardy told Human Rights Watch, “[H]istorically, most women go to the doctor for reproductive care because they are pregnant.… Once a woman gets beyond childbearing years, they don't go back to get Pap smears.”[233]
This is still the experience for some older women. Priscilla M., 75, of Sumter county, for example, started getting annual Pap tests in her early 30s.[234] She could not remember exactly when she stopped screening but said, “It’s been a long time.”[235] Her last Pap was sometime in the 1990s, when she was in her 50s. When asked about the reason for the gap, she said, “I know I should have [had a Pap test]. But I just didn’t.” If her doctor ever did recommend a Pap, Priscilla said she would do it because “at my age, I want to stay healthy.” Another older woman, Dolores A., 68, described an unclear screening history with no Pap test within at least five years.[236] She said that she had not been screened more recently because her doctor never recommended it.[237]
Most professional organizations recommend that women stop receiving cervical cancer screenings at 65. But that only applies to women with adequate screening history, including three consecutive normal Pap tests or two consecutive negative HPV tests within 10 years, with the most recent screening within five years.[238]
In three circumstances women may be clinically indicated to continue receiving screenings after 65 if a) they have not had three consecutive normal Pap tests, or two consecutive negative co-testing results, within ten years before stopping screening, the most recent test occurring within five years; b) they have had high-grade precancerous lesions within 20 years; c) the adequacy of their prior screening is unknown.[239]
Kira D., 71, of Greene county, falls into the first category.[240] She had an abnormal Pap test when she was 62 years old and uninsured. A repeat screening returned a normal result and she never went back for another. “Even after the first positive … well, abnormal Pap, then I went on and I was fine. You know because I retired at 62 [and lost my insurance]. This is going on 63, 64, 65. And then I got my insurance.”[241] At 65, Kira enrolled in Medicare and, despite having an abnormal screening history, was never re-screened. Two years later, she was diagnosed with stage II endometrial cancer after she noticed vaginal spotting.
The number of women, like Kira, who have “inadequate prior screening” is unknown but could be relatively high. Recent data suggests that one in every four women aged 45 to 64 years old have not been screened in the preceding three years.[242] This is especially concerning in light of CDC statistics showing rates of cervical cancer death rising steadily with age,[243] and evidence that older Black women in particular die from cervical cancer at exceptionally high rates in the US.[244]
IV. Cervical Cancer Care Is Limited by Lack of Access to Comprehensive Reproductive Health Care
Risk factors for cervical cancer include smoking, immunosuppression, coinfection with other sexually transmitted infections (STIs), like herpes, chlamydia and gonorrhea, and giving birth often or at a young age.[245] Women’s ability to control the number and spacing of their children is an important aspect of the management of cervical cancer risk factors. The state’s approach to reproductive health care, including abortion, its provider shortage, and its lack of public transportation options contribute significantly to an environment in which women die from cervical cancer at higher rates than in any other state in the US.
Alabama should do more to ease access to follow-up procedures and cervical cancer treatment by expanding Medicaid, supporting and working with pre-existing networks and resources, eliminating reproductive health restrictions, and easing the burden of transportation through better public transit options.
Alabama’s Climate of Hostility Around Aspects of Reproductive Health Care
A comprehensive approach to effective cervical cancer prevention—beyond HPV vaccines, screenings and colposcopies—requires policies that support women’s sexual and reproductive health and rights broadly, including autonomous decision-making about their reproductive future.[246] Alabama is among the states with the most abortion restrictions and some of the lowest scores on supportive policies and indicators of women’s health. [247] Moreover, recent developments have made the anti-abortion environment more prominent. The Alabama Constitution was amended in the November 2018 midterm elections to expressly state that 1) “it is the public policy of the state to recognize and support the sanctity of unborn life and the rights of unborn children” and 2) the right to abortion is not protected under the state constitution.[248] With the change, Alabama is poised to criminalize abortion care if the landmark abortion rights case, Roe v. Wade, is overturned or further eroded by the US Supreme Court. States that adopt more abortion restrictions tend to have fewer evidence-based policies to support women’s and children’s wellbeing overall.[249]
Comprehensive cervical cancer prevention and control should include access to the full spectrum of reproductive health information and services, including access to abortion and contraceptive information and services.
In the US, abortion care is increasingly becoming marginalized from mainstream medical care.[250] Access to safe, effective, and affordable contraception and abortion care are integral to the ability to control the number and spacing of one’s children. Yet many women must go outside of their normal health care system to obtain an abortion.[251]
Like many states in the US, Alabama targets abortion providers for heightened regulation. The non-evidence-based hyper-regulation of abortion-related care creates what a federal judge has called a “climate of hostility” around legal abortions in Alabama.[252] Currently, there are six laws in effect that target abortion providers. Women are required to undergo ultrasounds before abortions and abortion clinics must provide in-person, state-directed counseling, which includes information designed to discourage the recipient from having an abortion, at least 48 hours before the procedure.[253]
Such laws and policies restricting access to abortion services and information can create a “chilling effect” that suppresses the provision of safe, legal health services and deters women from seeking care.[254] They contravene the research-driven guidelines developed by the American College of Obstetricians and Gynecologists and the World Health Organization.[255]
Women who cannot access abortions when they need them are at a higher risk of poverty, serious physical impairment, mental anxiety, and intimate partner violence.[256] Supportive policies, on the other hand, have been shown to lead to improved health and safety, lower poverty rates, and better birth, developmental, and education outcomes for children.[257]
The Alabama state director for Planned Parenthood Southeast, a regional organization, told Human Rights Watch that:
The political landscape in Alabama is incredibly hostile to reproductive health and rights. Most recently, the Alabama legislature passed a bill that would pave the way to outlaw abortion in all circumstances—even in cases of rape, incest, and if the life of the woman is at risk. As a result of these kinds of attacks, we continue to rank among the 10 worst states in terms of women’s health. We are living proof of the dangerous consequences of anti-women's health policies.[258]
Alabama’s Policies or Practices Create Barriers to Cervical Cancer Services
The lack of obstetrician gynecologists is of pressing importance to reducing cervical cancer deaths in Alabama. It contributes to long travel times and makes access to care burdensome, costly, and impossible for some. The state’s obstetrician gynecologist shortage is disproportionately concentrated in the western portion of the Alabama Black Belt—where communities tend to be primarily African American, poorer, and in worse health than the rest of the state—and shifts the burden of transportation gaps on those least able to shoulder it. At the same time, the fear of stigma or misconceptions about local clinics make women less likely to seek care that is closer to home.
The Failure to Expand Medicaid Eligibility Helps Fuel Gynecologist Shortages
Colposcopies are more difficult to access than cervical cancer screenings in Alabama because they require a specialist. Fewer than half of the counties in Alabama have an obstetrician gynecologist and the counties without one are clustered in the central portion of the state.[259] Only 4 out of 17 counties in the Black Belt have an obstetrician gynecologist and the only low-income colposcopy clinic is in Birmingham, hours away from some counties.
Dr. Stevens, an obstetrician gynecologist in Selma, primarily caters to women who are uninsured or on Medicaid.[260] Fourteen of the surrounding counties are without a gynecologist. The next closest counties with gynecological hubs are Tuscaloosa to the north and Mobile to the south, leaving about a 200-mile area with no obstetrician gynecologist. This creates a high demand for Dr. Stevens and the one other obstetrician gynecologists in Selma.[261] The wait time can be immense and Dr. Stevens says he works for months without a break. “I was on call from November 5 of 2017 until March 16th of this year [2018] before the hospital brought somebody in for a week,” Dr. Stevens said. “Now I'll go from March 25th until the 9th of July before somebody comes in.”[262]
Many factors contribute to the obstetrician gynecologist shortage in rural America, including dwindling populations; high poor, uninsured and elderly populations; and providers’ personal decisions about where to live and practice. Obstetrician gynecologists provide medical and surgical care to women, specializing in pregnancy, labor, and the health of the female reproductive system. Therefore, along with regular visits involving preventive care or family planning checkups, obstetrician gynecologists are often also on call for emergency or unplanned procedures. As one doctor said, “You don’t want to be the only obstetrician gynecologist in a 150 mile radius. You’d never sleep!”[263] However, the most significant driver of the obstetrician gynecologist shortage is lack of hospitals with maternity services.[264]
It is difficult for rural hospitals to remain operational and obstetrician gynecologist programs have taken a particularly devastating hit.[265] In 1980, 45 of Alabama’s 54 rural counties had a hospital that provided obstetrics care.[266] By 2016, that number was down to 16, with only two counties covered in the traditional Alabama Black Belt. State and federal policies have deepened the crisis: experts and providers link the problem of rural hospital closures to Medicaid expansion decisions.[267] Hospitals in states that did expand Medicaid have seen increased coverage as well as decreased uncompensated care for uninsured people, and were shown to be substantially less likely to close than hospitals in states that did not expand their Medicaid programs.[268]
Not all gynecologists in Alabama are willing to take Medicaid patients, thinning out an already thin field. Reimbursement rates from the state are low—so low that, one ABCCEDP official told Human Rights Watch, “The crisis the medical field is in [low] reimbursement.”[269] A handful of community-minded colposcopy providers take on the lion’s share of diagnosing and treating ABCCEDP-eligible women at a loss. “We are always seeking more colposcopists or gynecologists than are willing to contract with us. So yes, we have trouble finding enough,” said the ABCCEDP official. “They’re the hardest ones to find of all of the providers.”[270]
The obstetrician gynecologist shortage makes it difficult for rural women to consistently access gynecological care and has negatively impacted women’s health-seeking behavior in the Black Belt. Many women whom Human Rights Watch interviewed did not have a regular gynecologist and instead sought one out only when potential reproductive health problem arose.[271] Others described driving between forty minutes and two-and-a-half hours for reproductive health care appointments or foregoing care altogether.[272] For some, it is easier simply to cross state lines.[273]
The Alabama government took a step towards identifying the barriers to care that contribute to gynecological cancer incidence, including cervical cancer, this year when it established the Alabama Study Commission for Gynecological Cancers.[274] The commission is comprised of medical specialists, researchers, patients, survivors, and advocates, none of whom are compensated for their time. It is tasked with reporting findings and recommendations to improve care and better address the unmet needs of Alabamians with gynecological cancer and their families to members of the legislature and the governor no later than March 5, 2019, at which time the commission will be disbanded. This is a step. However, without any mechanism to support implementation of the commission’s recommendations, it risks the same problems faced by the Alabama Health Care Improvement Task Force, when the recommendation to expand Medicaid was never implemented.[275]
Impact of Gynecologist Shortages and Lack of Adequate Public Transportation
The state’s failure to fund public transportation compounds the burdens that poor women must shoulder, lest they risk missing out on life-saving cervical cancer care. Alabama is one of five states in the US that fails to provide any state funds for public transportation.[276] Some cities maintain bus or transit systems through passenger fares as well as local and federal funds.[277] But ultimately, the system is highly fractured and mobility overwhelmingly dependent on cars.[278] In a state with a severe dearth of obstetrician gynecologists, long travel times are often part of the reproductive health care experience. Alabama should take positive measures to ensure that women in need of reproductive health care have transportation to those services.[279]
Alabama’s constitution by design limits public transportation funding. The logical and most common source for public transportation in the US is gasoline tax revenues.[280] By directing gasoline tax revenues to road and bridge construction only, a 1952 constitutional earmark effective closed off the natural funding stream for public transportation in the state.[281] “This does not leave a lot of other options or revenue sources for public transit,” said Jim Carnes, the policy director of ARISE Citizens’ Policy Project, “so we’ve had to fight, really fight, uphill on that question.”[282]
The meager forms of public transportation that do exist are not sufficient to fill the need. There are two main types: Medicaid non-emergency transportation or some local form of transit. The first only provides rides to health care appointments that are Medicaid-funded and includes other administrative hurdles, such as a five day advanced notice requirement.[283] As for local public transit systems, most counties in the Alabama Black Belt either do not have one or are served by West Alabama Public Transportation (WAPT). Because public transport options do not meet their needs, women commonly pay family, friends, or community members, from $15 to $70 to take them to an out-of-county gynecologist, which compounds the financial strain of seeking care.[284]
Friends or family had to take Cynthia H., 55, of Greene county, about 45 minutes each way to the closest medical hub in Tuscaloosa, for her colposcopy, hysterectomy, ovarian cancer-related treatments, and numerous non-gynecological surgeries.[285] She is unable to work and the cost of travel—sometimes multiple trips per week at about $50 per trip between 2005 and 2010—compounded the challenge of paying medical bills, household bills, and rent. When she couldn’t keep up, her electricity was shut off. “It was really hard.… I try not to let my rent get behind because even though I don’t have lights, I have a place to live.”[286]
Women who are on Medicaid or uninsured are often forced to travel longer distances because gynecologists who accept Medicaid or provide reduced-cost services are more limited. Darcy C., 57, of Choctaw county, who needs monitoring for a recurrence of endometrial cancer has to make a drive of two to two and-a-half hours to UAB every six months for a checkup, including a Pap test, with her gynecologic oncologist.[287] There are closer medical centers, but they only accept a certain percentage of Medicaid patients and she did not make the cut.[288] She pays up to $150 for transportation and the financial strain has forced her to forego non-essential expenses such as fresh food, although she wishes she could eat healthily while in treatment. “It’s hard. It’s really hard,” she said. “And I have to go without a lot to make sure that I have the money…, I get barely $700 a month, so with the bills I have to pay, it doesn’t leave anything for a trip.”[289]
Hazel B., 47, of Greene county, had to get to and from Demopolis, about 45 minutes, once a month; later, she had to travel to Birmingham, two hours away.[290] Without a job or insurance and with newly diagnosed breast cancer, Hazel relied on her family to pay most of her medical and transportation expenses, but she could not afford her mortgage.[291] Her home went into foreclosure, a legal procedure wherein the bank tried to reclaim her home, while she was waiting for approval for Alabama’s Medicaid for the disabled, a process that took three years.
I didn’t have any money to pay any bills…. So, I didn’t pay my house note and my house went behind and went into foreclosure. I didn’t want my uncle and them to try to pay my house note…. They couldn’t afford to pay it and pay medicine and help me get back and forth to the doctor and stuff like that.
The experience was psychologically draining. “You’re losing your house, you can’t pay your bills and this dollar, dollar. You got cancer. All this stuff rolling around in your head and your mind won’t shut down so you can’t sleep.”[292]
Without state support, women, providers, and community health advisors, described relying on “skills,” like soliciting donations, to connect women to care they would otherwise miss.[293] Health care workers told Human Rights Watch that they sometimes give patients money from their own pocket or drive them home if they’ve been left behind by the people who brought them there.[294] Indeed, sometimes Hazel was only able to get home because of the help that her doctor provided. “When I was doing the chemo, [my doctor’s office] would give me gas cards. And Dr. Shelby was real nice. He would give me money out of his pocket. He’d ask me if I had gas in my truck, and one day I didn’t. He reached in his pocket and gave me $60. He’s nice.”[295]
Kira D., 71, of Greene county, with stage IV endometrial cancer and two young children, told Human Rights Watch about the difficulties older people face.[296] “If you’re an elderly person— can’t drive and have to wait for someone to carry you—then they’re [the person driving] going to charge you over half of your paycheck,” she explained. “Then they don’t want to wait on you to finish your exam.”[297] Alabama has some of the highest senior poverty rates in the country.[298]
Amber W., a nurse at a local health clinic in Perry County, has older patients who are particularly vulnerable to missed appointments due to transportation concerns.[299] “Some people do not go to the doctor because they couldn't have anybody take them and they have to pay somebody crazy amounts to take them. They’re taking advantage of older patients,” she said.[300]
Rationing medication—deciding which medication is the least important or most expensive and forgoing it to pay for transport—is a common strategy. Odette M., 54, of Marengo county has had to cut back on medication in order to afford regular trips to Birmingham—about $60 to $70 and 3 hours—for Pap tests after an abnormal cervical cancer screening and follow-up treatment.[301] “I decide which one I got the most of, and which one is the important medicine. The one that I think I can get by [without] for a couple of weeks, I always cut back on that,” she told Human Rights Watch.[302] Paying for travel over medication put her “blood out of whack” and makes her doctor “fuss” but getting to Birmingham requires tough choices, such as not taking medication.[303]
In a positive development, Alabama recently passed a public transportation trust fund law, which created a repository for future state and federal funds to expand public transportation options. This is a step forward. However, at the time of writing, it was merely an empty bank account.
Misgivings and Misconceptions about Social Safety Net Care Diminishes Willingness to Seek Available Care Closer to Home
Health care should be free from all barriers, including negative stereotypes and lack of confidentiality, that interfere with access to sexual and reproductive health services care in Alabama’s safety net clinics, including negative stereotypes and lack of confidentiality.[304] Even if services like cervical cancer screenings are affordable and close to home, women described avoiding county health departments because they are not respectful places to receive care.
Alabama county health departments have an image of being only for poor children, pregnant women, and people who need STI care. UAB’s Director of Community Outreach for Minority Communities, Claudia Hardy, told Human Rights Watch:
The stereotype is that only poor, pregnant folks go over to the health department.… It’s not seen as a wellness facility for the poor, the disenfranchised. It's your last resort…. There are stereotypes; there's stigma. If anything, if the state could do anything, [it would be] to improve their public relations. Improve their image … but more importantly improve their customer service … make people feel valued when they come in. Don't disrespect them.[305]
By improving the quality of care, Hardy says, the state could help address some of the public image issues that make women more reticent to seek out care.
Multiple women who spoke to Human Rights Watch expressed relief when they had insurance coverage and could avoid the county health department. Vanessa T., 20, enrolled in Alabama Medicaid after becoming pregnant, so she chose to stop going to the county health department.[306] “The people around the [health department] office like to talk…,” she said. “I don't want to go. I'd rather go to the doctor I have on my insurance now.”[307]
Odette M., 54, of Marengo county, prefers driving to Birmingham, two-and-a-half-hour each way, instead of going to her county public health department.[308] “Nah, I didn’t feel comfortable with them…. I just didn’t like that.”[309] She gave an example of why she prefers an option that requires driving for hours: “When I was there [Birmingham] last week, [the doctor] came in and said, “’Would you feel comfortable if I was to bring a student nurse in?’ I said no and so she didn’t bring her in.”[310] Odette doesn’t believe that the public health department would have extended her the same courtesy.
Many women told Human Rights Watch about serious confidentiality concerns at the county health department. “A person go there and whatever's wrong with them be leaked out,” described Sammy B., 52, of Sumter county.[311] “[One doctor] talks so loud you can hear him telling a woman she got a venereal disease and she comes out of there looking stupid.”[312] Such experiences can undermine trust—an essential component of quality health care—and leave women feeling disrespected or reticent to return to the county health department. Kathy L., a community health advisor, has seen women return from the county health department upset. “Some of the ladies have come back and said, ‘They treat us like low class citizens. They lash out at us and they talk to us loud across the waiting room like we hard of hearing...’”[313] In the words of one woman, “People shouldn't have to feel embarrassed that they used the public health department.”[314]
Some women report more subtle concerns that changed their decision about where to access care. Laura J., a 40-year-old mother living with lupus, prefers driving an hour to Tuscaloosa rather than going to a local clinic in Sumter county.[315] Sumter does not have a gynecologist, so going to the one in Tuscaloosa avoids the need for a referral to that facility later. Beyond convenience, though, mistrust heavily factors into Laura’s decision.[316]
Lupus can cause false positives on syphilis tests—and did so for Laura years ago while she was a patient at the county health department.[317] She was concerned that her confidentiality may have been breached in the process of clearing the false positive.[318]
Nine time out of ten the people who work at local clinics are local people and I just don't want them in my personal space. I like my privacy…. It's just, you know, looks, whispers, things like that.... Silence can be very loud.[319]
Such distrust can extend to other forms of safety net health care as well—clinics with sliding scales or free services can be implicated. One nurse said that area residents sometimes derogatorily call the sliding scale clinic in her county the “poor people’s clinic” and think “you're not going to get good care if it's free care.”[320] Some people shared similar skepticism with Human Rights Watch. “I don't mean to put our clinics down...,” one woman said, “but sometimes with certain situations, it's like a band-aid.”[321] Another woman, 47, from Greene county, was uninsured for three years. “If you don’t have insurance and you can’t pay, [doctors] don’t want to see you. They just do the minimum amount.”[322]
The Alabama Department of Public Health should investigate and address concerns about confidentiality and quality of care. This could include creating a transparent process to assess complaints against county health departments and a response plan that, for example, requires adequate implicit bias, sensitivity and confidentiality training for all staff members. ADPH should also consider forming a partnership with private clinics to ensure that even those who feel uncomfortable at publicly funded clinics have an avenue for low-cost health care.
Missed Follow-ups
Too many women in Alabama are missing follow-up colposcopy appointments and this puts lives at risk. Dr. Stevens, whose Selma office is the closest referral site for low-income women for five or six counties in the Black Belt, sees this often. About half of the women referred to his clinic from public health departments do not make their follow-up appointments.[323] Women referred from other low-income clinics have better follow-up rates but not near 100 percent, he said.[324]
The University of Alabama at Birmingham’s Colposcopy Clinic has a slightly lower compliance rate.[325] UAB is the primary referral center in the state for women with abnormal cervical cancer screenings from the county health departments. Dr. Stevens’ practice might be the closest for many in West Central Alabama, but UAB is the highest volume referral center in the state. The colposcopy clinic is only open on Friday mornings and the no-show rate is consistently above 50 percent.[326] Dr. Warner Huh explained to Human Rights Watch why this is not surprising:
We have patients that drive three to four hours to get here. We have patients who use a bus to get here then they have to get out in time to take the bus home…. To put that in perspective, the no-show rates—you know we can have as many as 75 to 100 patients in a clinic over a four-hour session—the no show rate could be as high as 60 percent.[327]
To put this in perspective, 90 percent of women go to follow-up care through the ABCCEDP, which serves a similar, albeit much smaller, population as the county health departments.[328]
If the county health department refers a patient, the same county health department is ultimately responsible for checking up after missed appointment.[329] Guidelines require that staff call and send letters to women who misses their colposcopies.[330] The Alabama Department of Public Health, which oversees the county health departments,[331] is in the process of switching over to electronic medical records and, although individual county public health departments might keep track of missed referral appointments, the ADPH does not have that information.[332] This makes it impossible to track indispensable information in the prevention of cervical cancer such as from which county public health departments are women missing follow-up colposcopy appointments.
V. Poor Access to Information Negatively Affects Cervical Cancer Related Care
Women in Alabama lack access to information that is indispensable to making informed decisions about cervical cancer related care. Alabama does not have adequate policies and regulations in place to ensure that residents can access complete and accurate HPV prevention information, including about vaccination. It fails to regulate, monitor, or support policies and programs that ensure school-age children receive equal, accurate, and comprehensive sexual health education, which has been shown to decrease risk-taking in ways that would also reduce cervical cancer risks. These gaps contribute to the persistence of existing social barriers to accessing timely cervical cancer care to continue, negatively impacting mortality rates. Alabama is no longer funding those peer support and engagement programs that have successfully used community voices and knowledge to overcome such barriers.
International human rights treaties recognize the right to access health-related information. This has been interpreted as including education about all aspects of sexual and reproductive health.[333] Education can be a powerful determinant of health including in ensuring that women and girls have access to cervical cancer preventive care. The full realization of women’s right to health requires the removal of all barriers that interfere with access to sexual and reproductive health services, education, and information.[334]
Absence of State HPV Vaccine Policies Leave Women and Girls Uninformed
The HPV vaccine can prevent a vast majority of high-risk HPV infections before they have the opportunity to develop into cervical cancer.[335] Despite the proven effectiveness and safety of the vaccine, uptake in the US has been slow and Alabama’s vaccination rate trails behind much of the rest of the US.[336] In 2016, about 57.7 percent of adolescent girls and 39.4 percent of boys in Alabama had received the first round of the vaccine, putting Alabama in the bottom fifteen states in the nation for girls, and even lower for boys.[337]
Alabama’s Department of Public Health has made efforts to address low vaccination rates by setting progressive goals to increase the number of initiated and completed vaccinations. The most recent statewide Comprehensive Cancer Control Plan (“state plan”) included a goal of increasing the HPV vaccine completion rates by 46 percent, ideally having 80 percent of adolescents up-to-date by 2021.[338] However, Alabama has not implemented key policies that would support access to and information about the HPV vaccine that could improve vaccination uptake rates—including expanding Medicaid eligibility through the ACA, enacting school-entry programs for vaccination, and mandating comprehensive sexual health education.[339]
The last state plan (2011-2015) highlighted the need for “a statewide HPV Taskforce with community and legislative support to research the barriers to HPV vaccination.”[340] The ADPH, ABCCEDP, and Medicaid are part of the Alabama HPV coalition along with a score of other groups.[341] Additionally, the Alabama Comprehensive Cancer Control Coalition, which produces the state plan, has partnered with the ADPH and ABCCEDP to conduct public outreach campaigns, like distributing educational materials designed to encourage HPV vaccination to boys, girls, parents, and providers.[342] They have also collaborated with UAB to create strategies to promote and improve vaccination rates on campus.[343]
But this type of community support lacks substantive legislative support. Alabama has enacted only one supportive policy to increase HPV vaccination rates: Licensed pharmacists can distribute the vaccine.[344] The Alabama House considered a bill that would have required that parents be given information about the HPV infection and vaccination, but it failed to pass the committee stage and no similar measure to support HPV vaccination has been considered.[345]
Without supportive policies, providers carry a heavy burden to increase vaccine uptake. A number of experts who spoke to Human Rights Watch believe providers’ failure to recommend the vaccine is a significant problem in the state. [346] The CDC recommends that the HPV vaccine be presented just like other childhood vaccines that target preventable diseases.[347] Because HPV is known to be a STI, experts report to Human Rights Watch a reticence on the part of providers. “The link to sex,” one researcher explained, “is a common barrier in all the pediatricians, parents, nurses, and stakeholders.”[348]
Studies show that Alabama doctors are not unique in this regard. Providers feel uncomfortable recommending the vaccine for 11-year-olds and 12-year-olds and few recommend it for 9-year-olds or 10-year-olds.[349] One study found that some physicians profile their patients in terms of perceived risk of sexual activity.[350] In another study, one in four health care providers reported not routinely recommending the vaccine for girls, and more than half reported not doing so for boys.[351] The discomfort that some pediatric providers feel in talking about sex or STIs, or in challenging perceived parental hesitancy, has further contributed to inconsistencies in recommendations.[352]
State health agencies can help overcome this hesitancy with training to increase provider support for the HPV vaccination and improve the quality of provider recommendations.[353] Providers have reported needing support, such as parental education materials, public health campaigns, and instructions on framing the vaccine as a priority for cancer prevention.[354]
Completion rates in the state have improved from the 2009 baseline of 25 percent to 35.4 percent in 2016.[355] However, these numbers are still below state and federal goals and among adolescent girls the three dose vaccine completion rate has been relatively stagnant since 2013, hovering in the high 30s and low 40s.[356] One doctor told Human Rights Watch that children’s and parent’s knowledge of the vaccine remains low. There are “not too many [patients] asking about it.” He continued, “I’m not sure they are aware of it because it has not been televised or broadcast that children, both male and female, need it.”[357]
Some women told Human Rights Watch they were aware of the vaccine and reported having their children vaccinated.[358] A few women, however, were unsure whether or not they knew of the vaccine, or if they or their children were vaccinated.[359] One young woman, 22, said she had heard of the shot and might have gotten one in high school.[360] This is possible but unlikely because less than 1 percent of secondary schools in Alabama report administering the HPV vaccine and less than 20 percent provide students with referrals to providers—the lowest secondary school referral rate for HPV vaccinations in the nation.[361]
Romilda H., 59, who lives with her two young grandchildren, told Human Rights Watch that the children were “probably” vaccinated for HPV because they are up-to-date on their vaccines; however, she wasn’t sure whether the HPV had been included.[362] Alabama requires that all school-aged children receive certain vaccines, but the HPV vaccine is not one of them.
Sammy B., 52, of Sumter county, is a mother of five children, ages 19 to 31.[363] She had heard of the HPV vaccine but her children’s doctor never recommended it. Sammy did not have any of her children vaccinated but she believed her 19-year-old daughter might have received the shot on her own.[364] Sammy told Human Rights Watch that if a doctor had recommended doing so, she would have gotten her children vaccinated.[365]
Until October 2018, the HPV vaccine was not recommended for people over the age of 26. Prior to that, those who were not vaccinated before 27 lost the opportunity to be protected against most cases of genital warts, cervical cancer, and a host of other HPV-related cancers. Interviewees who did not know, or were unsure, about the HPV vaccine would have had numerous contacts with the health care system. That represents a missed opportunity to protect the women or their children from HPV-related cancers through vaccination—a missed opportunity that a strong provider recommendation or improved access to information could have prevented. With the recent FDA approval for individuals 27 to 45 years of age to receive the vaccine, those who missed receiving the vaccine at a younger age now have the opportunity for vaccination, but targeted outreach is needed to increase vaccination across age groups.
The last state plan acknowledged that the state faces an uphill battle because of the absence of supportive HPV vaccination legislation in Alabama.[366] State agencies have tried to work collaboratively with partner on strategies to improve awareness and uptake of the HPV vaccine.[367] But completion rates remain low and provider recommendation remains important. Deeanna M., 28, who has three young boys, ages 8 and 3 years, and 2 months, told Human Rights Watch that she might have heard about the vaccine, but her children’s doctor never discussed it.[368] There is still time for them and their generation. Alabama can save lives by enacting policies that increase provider, parental, and adolescent education about, and access to, HPV vaccinations.
Subpar Sexual Health Education in Schools Leave Children Unprepared
The state of Alabama does not provide the necessary guidance, funding, or accountability mechanisms to ensure that all students receive quality sexual health education. It puts the onus on individual school systems, many of which are already overstretched and underfunded. Moreover, the state’s education code actively inhibits local schools from providing comprehensive and inclusive sexual health education.
Access to full and medically accurate information about sexual and reproductive health is essential to secure the right to the highest attainable standard of health, and in the case of cervical cancer, access to information about preventive care could be lifesaving. But Alabama’s sexual health education falls short and leaves women and girls without the tools necessary to decrease cervical cancer risk. Furthermore, the state is missing an opportunity to combat understandable and persistent fears and social norms that inhibit women and girls from discussing or seeking sexual and reproductive health care, such as cervical cancer care.
The Flaws in Alabama’s Sexual Health Education Leave Women and Girls without The Tools Necessary to Decrease Cervical Cancer Risk
Alabama underfunds certain school systems because of the way education is funded, and because of limitations on the ability of state and local governments to raise revenue.[369] Amendments have resulted in agricultural and forest property being taxed at lower rates than most other property classes and given special exceptions.[370] Constitutional limitations on property taxes—as the source of all or most local funds for public schools—impact local revenue that would help pay for public schools.[371] Restricting locally imposed property taxes effectively restricts local officials’ ability to fund their public schools.[372]
According to an Alabama district court, it is “a vestige of discrimination inasmuch as the [state] constitutional provisions governing the taxation of property are traceable to, rooted in, and have their antecedents in an original segregative, discriminatory policy.”[373] Human Rights Watch spoke with Larry Menefee, a lawyer who challenged the discriminatory impetus and impact of Alabama’s property tax system in 2011 on behalf of public schoolchildren in the state. Because the Black Belt is a hub for agricultural and timber industries, its land and schools tend to be disproportionately—though not exclusively—impacted by low property tax income.[374] “This is such a barebones system…” Menefee explained. “These kids are starting with at least two-and-a-half strikes against them.”[375]
Similar to local school funding, sexual health education varies widely depending on the school district. Alabama does not have regulations in place to ensure that all students have equal opportunity to access sexual and reproductive health related information and advocates worry about the impact of the poor state of sexual health education in Alabama schools.
A vast majority of cervical cancer cases are caused by HPV, a sexually transmitted infection, and many cervical cancer risk factors, such as giving birth to multiple children or at a young age, having multiple sexual partners or living with HIV, are directly related to sexual activity.[376] Comprehensive sexual health education can address this head on, and has been shown to increase condom and contraceptive use; decrease likelihood of teen pregnancy, HIV or other STIs; delay the initiation of sexual activity; and reduce the number of sexual partners and sexual risk taking, such as unprotected sex—all of which would have the effect of reducing cervical cancer risk.[377] Indeed, the World Health Organization considers condom promotion and heathy sexuality education for boys and girls to be necessary tools for the prevention of cervical cancer.[378]
It is optional for schools in Alabama to teach sexual health education. But if a school does decide to offer sexual health education, the state’s education code sets the minimum content that must be included.[379] Advocates for comprehensive sexual health education say that the standards create value-laden guideposts that overemphasize abstinence, contain sex-negative language, stigmatize homosexuality, and require schools to teach about HIV prevention in medically inaccurate terms.[380]
The Alabama sexual health education standards are as notable for what they do not include as what they do. The state does not a) set a model curriculum for schools to follow; b) require that programs be medically or scientifically accurate or appropriate for students of all genders, sexual orientations and ethnic or cultural backgrounds; c) appropriate state funds specifically to support sexual health education; d) track which schools do or do not offer sexual health education, or what the curricula looks like at those that do.[381] In the words of one advocate, “The state is not even doing the bare minimum to provide sexual health education.”[382]
Contrast this with California, which does mandate comprehensive sexual health and HIV prevention education. The state a) provides curriculum guidance; b) requires that all information be medical accurate and appropriate for students of any race, gender, sexual orientation, ethnic, or cultural background, disability status, or level of English proficiency; c) provides block grants to fund mandated programs, like comprehensive sexual health and HIV prevention education; and d) requires that school districts train their teachers in the most recent medically accurate research on human sexuality, healthy relationships, pregnancy, HIV, and other STIs.[383]
According to Alabama Code § 16-40A-2, schools that teach sexual health education should include “age appropriate” information about the level of effectiveness that various contraceptive measures afford against STIs, while emphasizing that abstinence is the only completely reliable method. This language does not necessarily preclude comprehensive sexual health education.[384] Statistics, however, indicate that Alabama schools err towards less, rather than more, complete sexual health education. Only half of the high schools in the state teach students how to obtain condoms and fewer than half teach students how to use condoms correctly.[385] Only about 20 percent of Alabama schools teach sixth to eighth graders that preventive care is necessary to maintaining sexual and reproductive health—the second lowest rate in the nation.[386]
Without oversight of schools’ sexual health education curriculum, it is difficult to know which counties or school systems offer sexual health education, what that education looks like, or where the gaps are.
One consequence of inconsistent sexual health programs across the state is reflected in the rates of HIV and other STIs.[387] “In areas where sexual health education is weak or not offered, the rates [of HIV] are higher and you can see that especially when you drill down by age range…” said Alex Smith, the Executive Director of Equality Alabama. “The state’s dereliction of duty in this case is really telling—they just don’t care.”[388] The highest rates of new chlamydia infections and prevalence of HIV in the state are clustered in Black Belt counties, where Smith described the “biggest issues” talking about sexual health.[389]
Many counties contract with outside agencies, alleviating the need to develop their own sexual health program.[390] But some advocates say that the programs offered can be subpar and stigmatizing. “They’ll come in and say, ‘We have a whole program ready to go. All you have to do is contract us when you’re providing your sexual health courses and we’ll come in and take care of everything for you,’ which for our underfunded school system seems like a deal…,” said Matthew Pagnotti, the Director of Policy and Advocacy for AIDS Alabama, an HIV/AIDS service organization that has been involved in a statewide initiative to reform Alabama’s sexual health education system.[391]
But then [the contracted programs] provide horrifying experiences that stigmatize some of the youth in our state. Of the sentiments we’ve heard, a common one is that if you’ve had sex before, you’re a used, chewed up piece of gum and no one wants that. Or it’s like a piece of tape, and the more you use a piece of tape the less sticky it gets, the more it falls off of things and the less it works.[392]
Statistics confirm how far Alabama schools have to go. The CDC uses 19 sexual health indicators to test whether schools have the necessary components to achieve exemplary sexual health education that aligns with the National Health Education Standards.[393] In 2016, only 33.5 percent—or about one out of every three Alabama high schools—touch on all 19 topics in a mandatory course.[394]
A nurse from a Sumter county clinic told Human Rights Watch how the education system’s shortcomings can render programs that seek to improve health care access ineffective.[395] Free screenings, for example, are no use if women do not know when they should make use of them. “Often women come to the doctor when it’s already too late. They don’t know what the early signs are.… But if they were educated,” she went on to say, “they’d come more readily.”[396]
Lack of comprehensive sexual health education is also a missed opportunity by the state to challenge understandable and persistent social norms that make it difficult to discuss sex and prevent women and girls from seeking reproductive health care. Fear and embarrassment help drive silence and inaction in relation to cervical cancer care. “In some cases, there is a stigma or a shame. ‘That's my business and you don't need to know about my business’” said one nurse. “That's an issue, we really don't discuss sex."[397]
Frances Ford is the executive director of Sowing Seeds of Hope, a community building organization in Perry county, Alabama that advocates for better housing, employment, and health opportunities in the community.[398] Ford told Human Rights Watch that the women in her community seem more open about reproductive health concerns like HPV and cervical cancer. But progress still needs to be made.
Our culture is so different. Not talking about it is a cultural thing for African American women. Very limited on talking about female problems and issues. They keep it to themselves…. Now it’s not as much. I still think there are cultural barrier, but it’s better.[399]
Ford, who is African American, has firsthand knowledge of how devastating such norms can be. She lost her mother, Jeaneen, to cervical cancer and believes her mother delayed going to the doctor because she was uncomfortable doing so. “She knew something was wrong.… People didn’t talk about things like that.… Women, just, you know, they let it drag on for a long time before addressing it.”[400]
Fatalism is another problem. A nurse told Human Rights Watch, for example, that when refusing Pap tests, patients have told her, “I don’t want to know. I know I have an abnormal history,” or “I’m going to die from something…”[401]
Women, providers, experts, and advocates repeatedly expressed the need for better education to improve health outcomes in the Alabama Black Belt. “Education is key,” said a nurse at a Sumter county health clinic.[402]
Some women reported not knowing where they could access free or low cost reproductive health care services.[403] In a group interview with 18 women from Wilcox county, for example, the resounding response to a question about whether the county health department provided free Pap tests was “I don’t know.”[404] “A lot of people are not educated in the things they can have,” one of the participants added. “Like you said, free breast exams and Pap smears. They don’t know about it.… They just don’t know and it takes an entire community to get out and tell people about it.”[405]
Prevailing misconceptions about the public health department is a big part of the outreach problem. “There's not enough knowledge out in the community about what the health department can do,” UAB’s program director for community-based minority health programs told Human Rights Watch. “You still have people thinking it's just a family planning clinic.”[406] Darcy C., 57, of Greene county, for example, thought she did not qualify for services from the county health department:
I thought there was criteria that you had to meet, and I thought with me being married and not being a single mother or nothin’, I just didn’t know that I could go down there anyway and have my Paps and everything.
According to some interviewees, the outreach problem is made worse by uninformed staff who have incorrectly told women that they do not qualify for programs through which they could access a free screening, such as Plan First or the ABCCEDP.[407]
It is not clear how widespread the misinformation problem is. Claudia Hardy, UAB’s program director for community-based minority health programs, was responsible for establishing and training networks of community health advisors (CHAs) to help navigate more Black Belt women to breast and cervical cancer care.[408] Her staff know the eligibility requirements and know when someone is wrongfully turned away:
I hear it from my staff throughout the field who have more interaction with the public health department than I do. It's that the [health department] staff don't know their programs so that when people call, they can't direct them in the right way and they usually will turn people away.... The state health department needs to provide greater customer service, training for their staff.[409]
Kathy L., one of the staff members whom Claudia mentioned, has gotten on the phone after women told her that they were turned away both on the grounds of eligibility and more subjective grounds, like arriving late and then being denied the opportunity to reschedule a same-day appointment despite provider availability. “I’ve actually had to report them to their bosses to say, ‘Why is it that they don't want to see these ladies?’”[410]
ABCCEDP staff told Human Rights Watch that they have established an informal process for dealing with mistaken county health department staff.[411] If someone reports being wrongfully rejected, they call the county in question, reiterate the eligibility standards and ask them to remedy the situation.[412]
But not all women are willing or able to advocate for themselves and sometimes, Human Rights Watch found, the experience of being turned away is enough to stop women from returning. Nicole M., 56, of Lowndes county, is a full-time caregiver for her mother, who is 96 and a double amputee, and brother, who is 54 and a stroke survivor with Down syndrome.[413] She makes regular visits to her primary care physician but hasn’t has a cervical cancer screening in over 10 years.[414] In the past, she went to her county public health department for care. She says that one year a staff member told her that she would not qualify for a Pap until she was 50 years old.[415] She left and even though she is now older than 50, still has not returned. When asked why not, Nicole replied, “I just didn’t think about it.”[416]
The ABCCEDP found an efficient way to help combat such barriers to cervical cancer care: targeted information campaign. Women who had previously refused follow-up went, enabling the program to meet its quality assurance indicators and save lives. “Yes, it’s exciting that we met our measure, but the really exciting part is those are six women who really wouldn’t have come back...,” the program director told Human Rights Watch. “Those are six women that Dr. Huh isn’t going to find late-stage near the end and wish we’d caught them earlier.”
Community Outreach Programs Can Successfully Mitigate Some Barriers to Care, But Funding Cuts in Alabama Puts Them at Risk
The state has taken steps to improve community education and awareness. County health departments work with local partners to put on outreach events like health fairs and information sessions. The National Cancer Institute (NCI) and ABCCEDP have contributed funds to the University of Alabama at Birmingham (UAB) Cancer Center’s Community Health Advisor (CHA) program in the Black Belt. The CHA program is an academic, community engagement network of local women, trained to identify, recruit, educate and navigate others in their communities to cancer information and resources.
The CHA program, which has been referenced throughout this report, established peer support and engagement networks in the Black Belt to connect otherwise reticent women to care and help disrupt misgivings about the health care system. Studies show that the Community Health Advisor model effectively improves knowledge of cervical cancer, health care access, and quality of treatment, especially in medically underserved areas.[417] The goal is to use community voices and trust to overcome systemic harms and understandable yet harmful social norms in those communities that are most impacted by health disparities.
As one lady said to me so vividly, “Some things just is and they’ve always been.” And when you're living in these disenfranchised, impoverished, enslaved communities, there are things that just is.… They're powerless. As member of the communities have become educated, have gotten better jobs, and more resources, then they are exposed to a cultural climate that says “Okay. I can have more, I can push to be more.... I can go out of town to get health care.”[418]
The program lost federal NCI funding after 16 years, and then state funding in 2017. “Funding from the state has never been a priority except the past two years," explained Claudia Hardy, who runs the CHA program at the UAB Comprehensive Cancer Center. Unfortunately, due to funding cuts and priority changes, the ABCCEDP is no longer contributing to the CHA program.[419] Before the CHA program, the state was reportedly less successful in conveying the cervical cancer services that it offered. “Until Dr. Partridge's program [the CHA program] came through here,” one woman said, “I don't even think women knew that they could go to the health department to get mammograms and Pap smears and all that kind of stuff.”[420]
The CHA model uses an empowerment model that builds capacity of individuals to chip away at the difficult problem of distrust and alienation from reproductive health care. “The community health advisors is essential because it uses a model of trusted individuals in the local community … particularly when you're working in vulnerable communities...”[421]
At least one woman who spoke with Human Rights Watch likely would not have accessed cervical cancer screening or follow-up if not for the encouragement and support of a local community health advisor. Nola M., 59, of Marengo county, works at a popular fast food restaurant.[422] She had her first Pap test in about two decades in 2017 after her local community health advisor, Kathy L., convinced her that it was important. Nola was screened through a county health department.[423] She received a letter saying that her cervical cancer screening results were abnormal. She did not understand and thought she had cancer. “Man, I was like, ‘Oh Lord.’ I’m just fittin’ to die. I was just scared that that was it. When I brought her [Kathy L.] that letter, oh man.”[424]
Kathy L., a UAB Community Navigator, saw Nola crying at church “upset, crying, going up the alter asking for prayer. She was just really confused and upset.”[425] She helped explain what the letter meant and helped Nola schedule a follow-up appointment.
Uninsured, Nola was referred to UAB for a colposcopy.[426] No family members could take Nola to Birmingham so Kathy drove the two-and-a-half to three hours free of charge. Without Kathy’s outreach and navigational support, Nola likely would not have gotten follow-up care, potentially allowing her precancerous cells to develop into cervical cancer. “I don’t know. I was so scared,” she described, “Man, I’m talking about ‘Oh Jesus.’ I could see myself just dying. Just going to waste. If it weren’t for Kathy I don’t know what I’d do.”[427]
The CHA program is one successful method to empower community members to help educate their peers about breast and cervical cancer information and resources. Despite its promise in tackling the mistrust and disengagement with reproductive health care that continues to thrive in Black Belt communities, federal and state funding for the UAB CHA program are now at an all-time low, putting it at risk of ending.
VI. Legal Standards
The state and federal governments have allowed substantial barriers to comprehensive cervical cancer care to thrive in the state, and in doing so, has failed to protect women’s rights to health, information, and non-discrimination.
Right to Health
The International Covenant on Economic, Social and Cultural Rights (ICESCR) recognizes “the right of everyone to the enjoyment of the highest attainable standard of physical and mental health.”[428] The right to health entails health services, goods and facilities should be available, accessible, acceptable and of good quality, without discrimination.[429]The United States has signed but not ratified the ICESCR. However, this covenant is an authoritative interpretation of what the right to health entails and of the actions states should take in order to realize and protect it. The United Nations special rapporteur on extreme poverty and human rights recently asserted that health care is a human right in the US and that efforts to undermine the ACA “by stealth” are a violation of human rights.[430]
The Universal Declaration of Human Rights, which has the endorsement of all UN member states and is considered to be broadly reflective of customary international law, also articulates the right to health. The right to health is linked to provisions on the right to life, which is included in the International Covenant on Civil and Political Rights (ICCPR), which the US has ratified.[431]
Additionally, the right to health is contained in the Convention on the Elimination of All forms of Discrimination Against Women (CEDAW). The convention specifically addresses “the particular problems faced by rural women and the significant roles which rural women play in the economic survival of their families” and protects the right for rural women to have “access to adequate health care facilities, including information, counselling and services in family planning.”[432] The US has signed but not ratified CEDAW, and should regard the Convention as an authoritative guide to the steps it should take to realize and protect the rights of women, including their right to health.
Under the Universal Declaration of Human Rights, everyone has the right to a standard of living adequate for the health and well-being of one’s self and one’s family, including food, clothing, housing, medical care, and necessary social services, and the right to security in the event of unemployment, sickness, disability, widowhood, old age, or other lack of livelihood in circumstances beyond ones’ control.[433] The ICESCR establishes that medical care and necessary social services are integral components of human dignity and are part of the claims all people have to their right to an adequate standard of living.[434]
Right to Information, Including Effective Reproductive Health Information
Women and girls enjoy a right to access health-related information under numerous human rights treaties. This right includes access to reproductive health information, including that which is related to cervical cancer.[435]
Under the ICESR, the right to information requires states to provide complete and accurate information necessary for the protection and promotion of rights, including the right to health.[436] The Committee on Economic, Social and Cultural Rights, in its General Comment 14 has stated that the right to health includes the right to health-related education and information, including on sexual and reproductive health.[437] It also noted that “[t]he realization of women’s right to health requires the removal of all barriers interfering with access to health services, education and information, including in the area of sexual and reproductive health.”[438]
The CEDAW committee has noted that, under article 10(h) of CEDAW, women must have access to information about contraceptive measures, sexual health education, and family-planning services in order to make informed decisions.[439] In its General Comment No. 22, the Committee noted that “information accessibility includes the right to seek, receive and disseminate information and ideas concerning sexual and reproductive health issues…. All individuals and groups, including adolescents and youth, have the right to evidence-based information on all aspects of sexual and reproductive health…”[440] In particular, it has said that specific attention is needed to ensure that adolescent girls “have access to accurate information about their sexual and reproductive health and rights.”[441]
In the same vein, the UN Committee on the Rights of the Child (CRC), the expert body that interprets state obligations under the Convention on the Rights of the Child (another key human rights treaty the US has signed but not ratified), has called on states to ensure that children have access to reproductive and sexual education and information, including in schools.[442] In its General Comment No. 20, the CRC urged states to “adopt or integrate a comprehensive gender-sensitive sexual and reproductive health policy for adolescents, emphasizing that unequal access by adolescents to such information and services amounts to discrimination.”[443]
Right to Equality and Non-discrimination
Core international human rights treaties expressly prohibit discrimination and require the parties to these conventions to take measures to eradicate all forms of discrimination against individuals. The federal, state, and local governments in the United States are obligated to address all forms of racial discrimination, including disparities in reproductive health care, such as cervical cancer care. This duty is fundamental to upholding international human rights law, including the ICCPR and International Convention on the Elimination of all forms of Racial Discrimination (CERD).[444]
Under ICERD, the US undertakes to eliminate racial discrimination and guarantee to everyone, without distinction, the right to public health.[445] The treaty obligates governments to address not only intentional racial discrimination but laws, policies, and practices that result in disparate racial impact—that is, disproportionate negative effects on particular racial groups.[446] It requires governments, when the circumstances warrant, to take “special and concrete measures” to ensure the development and protection of racial groups “for the purpose of guaranteeing them the full and equal enjoyment of human rights and fundamental freedoms.”[447]
The UN Committee on the Elimination of Racial Discrimination, the international expert body responsible for monitoring implementation of CERD by its State parties, expressed concern in 2014 that the United States lacks appropriate mechanisms for implementation of the treaty at the federal, state and local levels. The Committee noted that “many states with substantial numbers of racial and ethnic minorities have opted out of the Medicaid expansion programme … thus failing to fully address racial disparities in access to affordable and quality health care.” It went on to specifically highlight the problem of racial disparities in the field of sexual and reproductive health. “It also reiterates its previous concern at the persistence of racial disparities in the field of sexual and reproductive health, particularly with regard to the high maternal and infant mortality rates among African American communities.” [448]
The committee recommended that the US take “concrete measures to ensure that all individuals, and in particular racial and ethnic minorities who reside in states that have opted out of the ACA … have effective access to affordable and adequate health-care services.” The findings in this report show that the US has not successfully fulfilled that recommendation.
Additionally, CESCR General Comment No. 20 on non-discrimination in economic, social, and cultural rights, recommended that states parties adopt:
Specific legislation that prohibits discrimination in the field of economic, social and cultural rights. Such laws should aim at eliminating formal and substantive discrimination, attribute obligations to public and private actors and cover the prohibited grounds discussed above. Other laws should be regularly reviewed and, where necessary, amended in order to ensure that they do not discriminate or lead to discrimination, whether formally or substantively, in relation to the exercise and enjoyment of Covenant rights.[449]
Even though the US is not a party to the ICESCR, it should consider the committee’s views as a useful and authoritative guide to the policies that governments should pursue in order to protect and realize the right to health.
Acknowledgments
This report was researched and written by Kelly Flannery, New York University School of Law Fellow in the Women’s Rights Division of Human Rights Watch. Amanda Klasing, senior researcher in the Women’s Rights Division, provided additional research support. Brian Root, quantitative analyst in the Program Office, provided quantitative data analysis.
Amanda Klasing edited the report. It was reviewed by Megan McLemore, senior researcher in the Health and Human Rights Division; Diederik Lohman, director of the Health and Human Rights Division; Bethany Brown, researcher on Older Person’s Rights, Disability Rights Division; Jasmine Tyler, advocacy director in the United States Program; Sarah St. Vincent, researcher and advocate in the United States Program; Bede Sheppard, deputy director in the Children’s Rights Division; and Brian Root, Quantitative Analyst. Christopher Albin-Lackey, senior legal advisor, provided legal review. Tom Porteous, deputy program director, provided program review.
Production assistance was provided by Tabashshum Islam, associate in the Women’s Rights Division; Jessie Graham, senior multimedia producer; Fitzroy Hepkins, administrative manager; and Jose Martinez, senior administration coordinator.
This report would not have been possible without invaluable guidance and support from groups and individuals with our project design, research, and advocacy. We are grateful to the reproductive health, rights and justice groups, nationwide, statewide and local advocates, community organizations, academic researchers, and medical professionals whose expertise helped shaped the direction, and deepen the quality, of the research and analysis presented in this report. In particular, thank you to those who allowed us to connect to and learn from networks of community members in the Alabama Black Belt, including Claudia Hardy, Isabel Scarinci, Pilar Ricon-Hernandez, Katie Glenn, Frances Ford, Deborah Clarke, Mel Prince, Laurie Dill, Felicia Lucky, Mary Moore, the women from the National Council of Negro Women, and the Wilcox County Human Rights Commission.
Finally, we are profoundly grateful to the women who shared their experiences and time with us and the community health advisors, including Glenda James, Kathy Levy, and Darlene Robinson, who acted as our research partners.