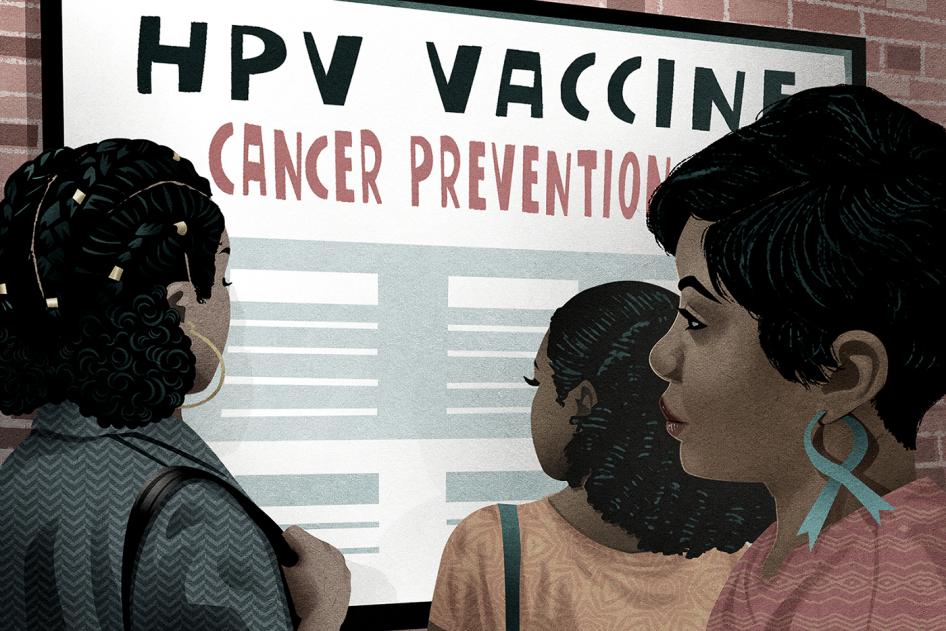
Since being approved by the US Food and Drug Administration in 2006, a generation of young women has received the HPV vaccine, which prevents almost all cases of cervical cancer. And earlier this year, the American Cancer Society reported some heartening news: From 2012 to 2019, incidence rates of cervical cancer dropped 65 percent among women in the US in their early 20s. And overall cancer mortality rates in the US have dropped by over 30 percent among all ages since 1991.
But the American Cancer Society also revealed a harsh truth. The report highlights the roles that structural racism, discrimination, and inequality play in driving these stark racial disparities. They affect exposure to cancer risk factors and access to equitable and high-quality care needed to prevent, detect, and treat cancer.
Cervical cancer is highly preventable and treatable and if caught early, the five-year survival rate is over 90 percent. Despite this, an estimated 4,290 people died of cervical cancer in the US in 2021. And Black women were more disproportionately represented in that number than any other racial or ethnic group. Black women have a higher risk of being diagnosed with cervical cancer at a late stage and have lower survival rates compared to white women for every stage of diagnosis, including when they are diagnosed early. Black women are also less likely to receive high quality and aggressive treatment for cervical cancer.
Since 2018, Human Rights Watch has documented barriers that are fueling racial disparities in cervical cancer death rates in rural communities in the South, first in Alabama and then more recently in Georgia in partnership with the Southern Rural Black Women’s Initiative for Economic and Social Justice.
Our research points to clear patterns of neglect, exclusion, and discrimination that prevent Black women in rural and underserved communities from accessing affordable, comprehensive, and equitable reproductive health-care services and information. Our research also shows that the US government and state governments can help eliminate these inequalities.
We spoke with women in Alabama and Georgia, the majority of whom were uninsured and living in poverty, who described how they couldn’t afford to pay for cervical cancer care. They said they often had to make difficult choices, sometimes choosing between buying groceries or paying their utility bills or getting the health care they needed. Although she was insured at the time we spoke with her, Tara, a pseudonym, 61 from Wilcox County, Ga., was unemployed and sometimes struggled to afford co-payments to see the doctor. In addition to rescheduling appointments at times when she couldn’t afford the cost, she said that sometimes she had to decide whether to pay her medical bills or buy food: “Well, sometimes it's a bill, or sometimes it's food. I leave out certain food.” This situation is common for uninsured, low-income people living in states like Alabama and Georgia that haven’t expanded Medicaid.
Many of the women we interviewed also reported not having adequate information on their sexual or reproductive health, including steps they could take to prevent cervical cancer through routine screenings and the HPV vaccine. In mostly rural communities, people told us repeatedly that this lifesaving information wasn’t available.
Women also found it hard to even see a gynecologist, sometimes having to travel to neighboring counties to visit one. Finding someone to drive them to appointments, paying for gas, and taking time off work are all challenges when the nearest gynecologist is over an hour away. This makes gynecological care burdensome and sometimes impossible to access for many women.
Women also described callous treatment, demeaning experiences, and instances when providers did not properly listen to their health concerns or provide an adequate level of care due to racial bias and discrimination.
When she was in her late 30s, Denise, a pseudonym for a 54-year-old woman from Wilcox County, Ga., started experiencing intense pain and heavy bleeding during menstruation. She also started receiving abnormal Pap test results. Denise had no idea what was going on and her gynecologist at the time did not explain the issue nor the plan to treat her, instead telling her that abnormal Pap tests happen all the time and “it's probably just fine, we'll just check it again.” After years of abnormal test results, Denise felt like she wasn’t getting proper care and sought out several new gynecologists.
“I went all over the state of Georgia trying to get help,” she said. Denise described interactions with a gynecologist who treated her poorly and used abusive language toward her, before she eventually found a new gynecologist who diagnosed her with uterine fibroids, which required a hysterectomy. The new gynecologist “said it wouldn't have been so bad if I had caught it earlier, because it was like my uterus was full of fibroids. It was just bad. If I'd caught it sooner, my surgery wouldn't have been so invasive.”
Such mistreatment further alienates some Black women from getting the reproductive health care they need and makes them reluctant to seek out services.
US federal and state governments need to address and eliminate barriers driving cervical cancer deaths and racial disparities in outcomes, including by expanding Medicaid and enacting policies to ensure affordable, accessible, and equitable cervical cancer care for all women, including those living in rural and underserved communities. The government should also ensure that everyone has access to information on their sexual and reproductive health, including information on the HPV vaccine, by mandating comprehensive sexual health education in all schools.
While the American Cancer Society report offers promising news, we must also acknowledge that Black women are more likely than others to die from cancer as a result of racism, discrimination, and inequality. The racial disparities we see in cervical cancer outcomes are an example of the ways that racial discrimination perpetuates health inequalities in our country. US federal and state governments need to take steps to dismantle racism and address the ways that discrimination and inequality impede the rights to health, information, and equality for everyone.